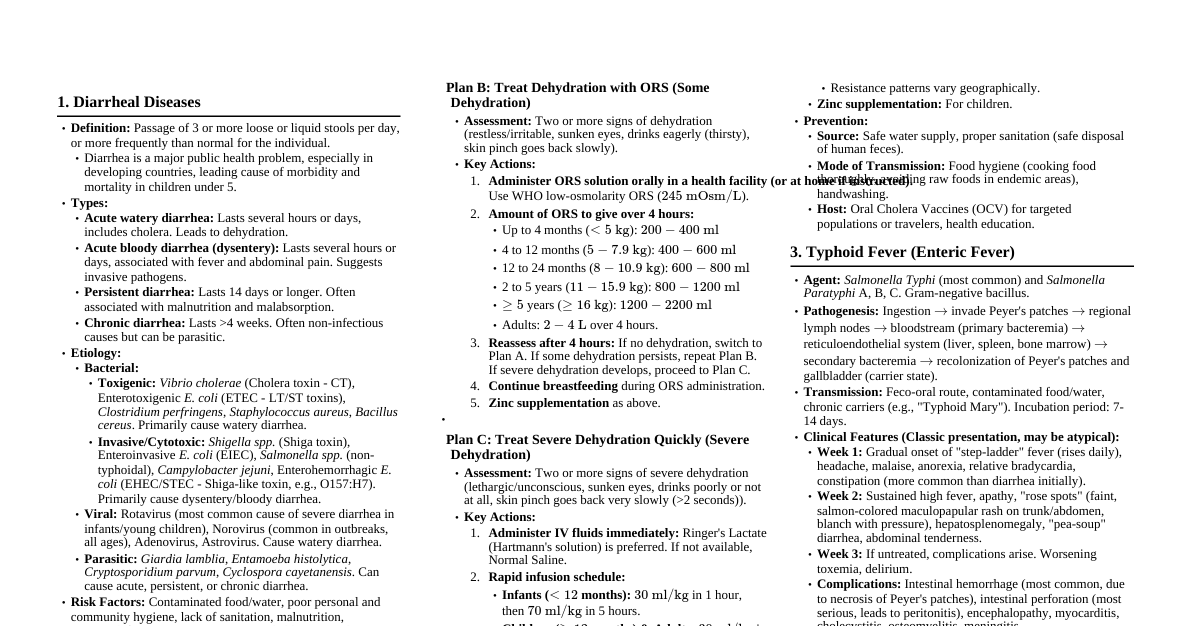
Diseases of the Urinary Tract Common Urinary Symptoms Difficulty in micturition, retention, and incontinence of urine. Acute Urinary Retention: Sudden inability to void, causing discomfort and pain. Often requires catheterization. Haematuria: Blood in urine, especially in elderly women, smokers, or those with chemical exposure, raises suspicion of bladder cancer. Causes of Acute Retention of Urine (Gynaecology) Category Causes Postoperative Oedema, reflex spasm of bladder sphincter, denervation (e.g., Wertheim's hysterectomy), spinal/epidural anaesthesia. Puerperal Bruising of vagina, painful perineal wound, inability to appreciate bladder filling. Obstructive Cicatrical stenosis (bladder neck surgery), inflammatory stenosis (gonorrhea - rare), sling operations (over-enthusiastic), cancers (cervix, vagina, bladder, urethra). Space-Occupying Lesions Haematocolpos, retroverted gravid uterus (12-14 weeks), haematocele (ectopic), cervical/uterine myomas, ovarian neoplasm (impacted). Neurological Spinal cord lesions, disseminated sclerosis, tabes dorsalis, bladder denervation (extensive surgery), anticholinergic/antidepressant drugs. Chronic Retention Bladder neck narrowing due to senile changes in urethra (old women). Treatment of Urinary Retention Address primary cause (e.g., remove organic lesion). Retroverted Gravid Uterus: Slow bladder emptying via indwelling catheter (12-14 hours), patient lies face down. Urethral Syndrome Symptoms: Dysuria, frequency, occasional stress incontinence; sterile urine. Causes: Oestrogen deficiency (postmenopausal), probable infection (young women: tubercle bacilli, Chlamydia). Treatment: Vaginal oestrogen cream (postmenopausal), appropriate antimicrobials (young women). Difficult Micturition Causes: Conditions leading to retention, bladder growth, urinary calculi, severe prolapse of anterior vaginal wall/procidentia. Mechanism: Straining causes further prolapse, urine forced into cystocele. Treatment: "Splinting" (digital manipulation), anterior colporrhaphy, pelvic floor repair, vaginal hysterectomy if indicated. Painful Micturition (Dysuria) Causes: Vesical origin (infection, bladder spasm), urethral origin (urethritis, caruncles, prolapse of urethral mucosa, vulval disease). "Honeymoon cystitis" (recent intercourse trauma). Cystitis (pain at end of micturition due to inflamed surfaces). Papilloma, carcinoma, tuberculosis, stone. Radiation cystitis (severe, small capacity, irritable bladder post-radium treatment). Investigations: Urine exam, culture, cystourethroscopy. Increased Frequency of Micturition Voiding >8 times/day or >1 time/night. Causes: Nongynaecological: Diabetes mellitus/insipidus, polyuric phase of renal failure. Gynaecological: Cystitis (E. coli, TB, stone, growth), early pregnancy, late pregnancy (presenting part pressure), pelvic tumours (myomas, ovarian cysts), cystocele (incomplete emptying), inflammatory swellings (parametritis, inflamed appendages), carcinoma of cervix/vagina. Retention overflow (overdistended bladder). Bladder neurosis. Investigations: Gynaecological exam, urine analysis/culture, cystoscopy, IVP, ultrasound. Treatment: Psychotherapy, bladder discipline, sedatives. Address underlying organic lesion. Incontinence of Urine True/Complete Incontinence: Continuous, involuntary discharge. Causes: Vesicovaginal/ureterovaginal fistula, malformations (ectopia vesicae, ectopic ureter), spinal cord diseases. False/Partial Incontinence: Nocturnal Enuresis: Voided during sleep (young girls). Stress Urinary Incontinence (SUI): Small quantities involuntarily with sneezing, coughing, laughing. Associated with anterior vaginal wall prolapse. Common in pregnancy/puerperium. Urge Incontinence: Strong, sudden desire to pass urine; if not quick, large involuntary loss. Due to detrusor instability. Cystitis Aetiology: Microorganisms: E. coli (most frequent), Klebsiella, streptococci, staphylococci, Bacillus proteus, tubercle bacilli, Pseudomonas pyocyanea. Catheterization: Most common cause of lower UTI (80% incidence post-gynaecological surgery). Descending Infection: From kidney (renal TB, chronic pyelonephritis). Adjacent Structures: Inflamed cervix, parametritis. Haematogenous/Lymphatic Spread: From genitalia or bowel. Symptoms: Painful/frequent micturition, bladder pain, strangury, pus in urine. Acute cystitis is severe (sleep deprivation, fever). Chronic cystitis has less pain/strangury but persistent frequency/pyuria. Diagnosis: Symptoms, urine exam. Differentiate from urethritis (pain during vs. end of micturition, abdominal pain/tenderness absence). Three-glass test. Treatment: Urinary antiseptics (nitrofurantoin, norfloxacin, ciprofloxacin, pefloxacin, sparfloxacin). Large fluid intake (2.5 L/24h), alkaline drinks. Bed rest (acute phase), hot water bottle. Spasmolytics (codeine, belladonna), citrates. Antibiotic sensitivity testing. Pyelonephritis (Pyelitis) Definition: Upper urinary tract infection involving kidneys, often complication of lower UTIs. Aetiology: Ascending infection from postoperative/puerperal cystitis, E. coli (pregnancy), advanced carcinoma of cervix/vagina (ureteric involvement/obstruction). Symptoms: Loin pain/tenderness, high temperature, rigors, headache, vomiting, furred tongue, frequency (associated cystitis). Affected kidney exquisitely tender (acute). Diagnosis: Turbid urine, pus cells, bacteria. Toxaemia, raised blood urea, casts in urine (acute). Treatment: Bed rest (unaffected side), copious fluids, systemic antibiotics (10-14 days), referral to urologist if unresponsive/recurrent. Diseases of the Female Urethra Urethritis Aetiology: Sexually transmitted: Gonococcus, Chlamydia trachomatis, Trichomonas, Candida, viruses. "Honeymoon cystitis" (coital injury). Oestrogen deficiency (menopausal women). Chemical/allergic reactions (deodorants, douches, contraceptives, tampons). Symptoms: Frequency, dysuria (pain during micturition, not at end). Inflamed urethral orifice, purulent discharge. Treatment: Appropriate antimicrobials, adequate fluid intake, vaginal oestrogen cream (menopausal), avoid irritants. Urethral Caruncle Definition: Swollen, congested posterior urethral mucosa, pouting like a cherry. Common in postmenopausal women. Symptoms: Postcoital bleeding, dyspareunia, pain, dysuria. Diagnosis: Exclude genital tract malignancy (cytology, endometrial histology, sonography). Treatment: Diathermy excision. Oestrogen (systemic or local cream) to aid recovery. Urethral Prolapse Definition: Prolapse of urethral mucosa. Aetiology: Chronic straining, oestrogen deficiency. Seen in very young and old. Treatment: Surgical excision of excess mucosa, suturing. Urethral Diverticulum Symptoms: Nonspecific (frequency, dysuria, dyspareunia, dribbling, urgency/incontinence). Swelling in urethral region. Differential Diagnosis: Urethrocele, Gartner's duct cyst, Skene's gland abscess. Treatment: Antibiotics, surgical excision or marsupialization. Complications: Urethral stricture, fistula. Urethral Stenosis Sites: Bladder neck, meatus. Aetiology: Congenital, infection, injury, neoplasm, diverticulum. Symptoms: Poor stream, straining, repeated UTIs. Diagnosis: Urethroscopy (narrowing, trabeculation). Treatment: Infection control, surgical removal of cysts/tumours. Intermittent urethral dilation, urethrotomy, reconstructive urethroplasty. Urinary Fistulae Definition: Abnormal epithelialized tracts between genital and urinary tracts. Aetiology: Developing Countries: Obstetric (prolonged/obstructed labor, difficult deliveries). Developed Countries: Operative trauma (pelvic surgery). Advanced genital tract malignancy. Radiation therapy (tissue necrosis). Types of Urinary Fistulae Vesical Fistulae: Vesicovaginal, vesicocervical, vesicouterine, vesicoabdominal, vesicointestinal. Ureteric Fistulae: Ureterovaginal, ureteroabdominal. Urethral Fistulae: Urethrovaginal. Clinical Features Bladder Fistula (VVF): Continuous dribbling, inability to pass urine. Ureteric Fistula: Continuous dribbling, but can also micturate. Urethrovaginal Fistula: Incontinence only during micturition. Vesicovaginal Fistula (VVF) Causes: Obstetric (difficult childbirth), post-hysterectomy. Symptoms: Constant dribbling (true incontinence), excoriation of genital areas, depression. Diagnosis: Visual inspection (knee-chest position, speculum), bimanual exam, methylene blue test. Management: Immediate post-delivery: Indwelling catheter (3-4 weeks), antibiotics. Established fistula: Wait 3 months for tissue recovery. Surgical repair: Vaginal approach (Latzko, Chassar Moir techniques), transabdominal (for large/complex fistulae, failed vaginal repair). Urinary diversion: Ileal loop bladder, rectal bladder (for extensive tissue loss, radiation fistulae). Postoperative: Continuous bladder drainage (14-21 days), antibiotics, no vaginal exams/intercourse for 2 months. Caesarean section for future pregnancies. Ureteric Fistula Causes: Direct injury or devascularization during gynaecological surgery (e.g., Wertheim operation). Congenital (rare). Symptoms: Transection: Immediate urinary leak into peritoneal cavity (nausea, vomiting, abdominal distension, ileus, fever, leucocytosis, loin pain). Ligation (bilateral): Anuria, flank pain, tender enlarged kidneys. Necrosis: Delayed leak (2 weeks+), dribbling from vagina, oliguria. Late Complications: Stricture, hydronephrosis, infection. Management: Early detection: Remove ligatures, stent ureters. Delayed diagnosis: Percutaneous nephrostomy (PCN), later reimplantation. Transection: PCN, retrograde dye injection, cystoscopic stenting (partial), repair surgery (complete). Surgical options: Ureteroureteral anastomosis, ureter implantation into bladder, Boari flap ureteroneocystostomy. Prophylaxis: Trace ureter during difficult surgery, medial dissection to preserve blood supply. Vesicouterine Fistula Causes: Caesarean section, uterine rupture, placenta accreta. Symptoms: Cyclical haematuria (Youssef syndrome), continent. Diagnosis: Cystoscopy, methylene blue into uterine cavity. Treatment: Prolonged catheterization (occasional closure), abdominal repair (omentum/gracilis graft). Urethrovaginal Fistula Symptoms: Continent, but dribbles urine only during micturition. Diagnosis: Speculum exam. Treatment: Vaginal repair (may cause stricture). Graft technique for large fistulae. Causes: Surgery for paravaginal cyst/urethral diverticulum, penetrating injury. Stress Urinary Incontinence (SUI) Definition: Involuntary leakage of urine with increased abdominal pressure in absence of detrusor contraction. Small amount. Prevalence: 25-40% of women, more common >40 years. Aetiology: Anatomical changes: Urethral hypermobility (80%), loss of posterior urethrovesical angle, sphincteric dysfunction. Age, multiparity, obesity, smoking, prolapse, constipation. Pregnancy/puerperium (progesterone effect, bladder neck descent, pudendal nerve denervation). Hereditary (collagen tissue loss). Post-VVF repair, urethral fibrosis. Mechanism of Female Urinary Continence Internal sphincter at bladder neck, urethral closure pressure ($P_{urethral} - P_{vesical}$). Normal closure pressure >20 cm H$_2$O. Urethra and bladder neck above levator ani muscles, urethrovesical angle >100°. Abdominal pressure transmitted equally to bladder and urethra. Atony of pelvic floor/pudendal nerve damage leads to bladder neck descent, loss of angle. Urge Incontinence Involuntary escape of large amount of urine following a strong desire to void. Often due to detrusor muscle overactivity (detrusor instability, DI). Sensory urgency (intense desire without detrusor pressure). Unconscious incontinence (neuropathic bladder, retention with overflow). Primary Clinical Evaluation History: Differentiate SUI (single spurt with physical exertion) from urge incontinence (strong desire, large loss). Relevant medical history (diabetes, pulmonary disease). Physical Examination: Pelvic/speculum exam, neurological assessment. Assess pelvic support defects, levator muscle tone, urethral mobility, vaginal wall prolapse, senile vaginal changes. Grading of SUI Grade I: Only with severe stress (coughing, sneezing, jogging). Grade II: Moderate stress (fast walk, stairs). Grade III: Mild stress (standing). Types of GSI (Surgical Perspective) Type I: Loss of posterior urethrovesical angle alone. Type II: Loss of posterior urethrovesical angle + urethral hypermobility. Type III: Intrinsic sphincter deficiency. Investigations Urine analysis, urine culture (mandatory before invasive procedures). Stress Test: Patient voids, catheterized, 250 mL saline instilled. Cough/strain while squatting on absorbent pad. Net weight gain >2g indicates GSI. Cotton Swab Stick Test: Swab in urethra, patient strains/coughs. Angle >20° above horizontal indicates bladder neck descent. Marshall's and Bonney's Test: Bladder neck elevated digitally or with instrument. Absence of leakage on straining/coughing indicates positive test (beneficial outcome from surgery). Urethroscopy: Visual evaluation of urethra, trigone, bladder neck. Provides information on opening pressure, urethritis, diverticulum, rigid urethra. Urodynamic Evaluation: Cystometry: Measures bladder/urethral pressures during filling. Differentiates SUI, DI. Normal: Uroflowmetry: Measures urine flow rate and volume. Normal: 15-25 mL/s. Micturition Cystourethrography: Shows urethrovesical angle. Uroprofilometry: Measures dynamic urethral pressures. Gold standard for GSI. Ultrasound: Bladder volume, residual urine. Bladder wall thickness >6mm suggests DI. Videocystourethrography: Combines pressure studies with video. MRI: Studies pelvic floor muscle defects and fascia. Neurophysiological Testing: For suspected neurological component. Treatment of SUI Conservative Treatment (First Line): Physiotherapy: Kegel pelvic floor exercises (4-6 months), electrical/magnetic stimulation. Drugs: $\alpha$-adrenergic drugs, oestrogen cream (menopausal), venlafaxine, imipramine. Intraurethral/Vaginal Devices: Ring pessary, vaginal cones (Contiform). Artificial Urinary Sphincter (AUS): For neurological conditions, previous surgical failure. Lifestyle: Weight loss, reduced caffeine, smoking cessation, bladder training. Surgical Repair (If conservative fails): Goals: Reposition proximal urethra, preserve urethrovesical angle, preserve urethral compressibility/pliability, preserve sphincter integrity. Vaginal Operations: Anterior colporrhaphy (Kelly's repair), Pacey's repair. Abdominal Operations (Retropubic Colposuspension): Marshall-Marchetti-Krantz (MMK), Burch colposuspension. Combined Abdominal and Vaginal: Pereyra operation. Slings: Fascial slings, nylon mesh slings, tension-free vaginal tape (TVT), transobturator tape (TOT). Periurethral Injections: Collagen, micronized silicon rubber particles (uroplasty, Durasphere, Bulkamid). Complications of Surgery: Injury to bladder/urethra, haematoma, infection, suture breakdown, voiding difficulties, erosion of sutures, DI. Detrusor Instability (DI) Definition: Detrusor muscle contracts spontaneously or on provocation during filling phase. Aetiology: Functional/psychosomatic, detrusor hyperreflexia (neuropathy: diabetic, CVA, MS, spinal injury, Parkinsonism), post-GSI surgery (bladder neck too high/tight), idiopathic, urinary infection. Symptoms: Involuntary urine escape with urge, frequency (>7 times/day, >1 time/night), bedwetting, incontinence during intercourse/with sound of water. Investigations: Neurological exam, blood sugar, urine culture, cystometry (pressure >15 cm H$_2$O at 200 mL), ultrasound (thick bladder wall >6mm, residual urine). Treatment: Lifestyle: Low caffeine, avoid smoking, bladder training, restricted fluid intake, weight reduction. Medical: Anticholinergic drugs (flavoxate, dicyclomine, propantheline, oxybutynin, imipramine, tolterodine, duloxetine, solifenacin, darifenacin). Other: Posterior tibial nerve stimulation (PTNS), transvesical phenol injection (short-term benefit), acupuncture, urethral dilation. Surgical (last resort): Augmentation cystoplasty (high cure, but complications: self-catheterization, infection, stones, malignancy). Botox (Botulinum toxin A) injection: Inhibits acetylcholine release, increases bladder capacity, effects last 9-12 months. Risks: retention, infection. Detrusor myectomy. Desmopressin (DDAVP) for nocturnal enuresis. Genital Tract Injuries Obstetric Injuries Most common type of injury. Circular fibers of external cervical os torn laterally. Hymen becomes carunculae myrtiformes. Superficial 1st-degree perineal lacerations are common. Severe lacerations of perineum are common. Vaginal tears from instrumental delivery or extension of perineal/cervical tears. Cervical lacerations from strong uterine contractions, occiput posterior position, cervical dystocia. Vesicovaginal fistula from ischemic necrosis or difficult forceps delivery. Rectovaginal fistula from complete perineal tear or suture. Extensive vaginal laceration can cause fibrosis and narrowing. Uterine rupture (high maternal mortality). Perineal Tears Thorough inspection of perineum and lower genital tract post-delivery is mandatory. Small non-bleeding lacerations can be left alone; others require surgical repair. Risk Factors: Big baby, prolonged labor, occipitoposterior malposition, instrumental delivery, breech, midline episiotomy, rapid stretching, rigid perineum. Prevention: Support perineum, gradual egress of presenting part, timely episiotomy (especially with instrumental/breech delivery). Caesarean section for previous complete perineal tear or difficult prolapse. Grading: First Degree: Skin of fourchette. Second Degree: Muscles of perineal body. Third Degree: Extends partially through external anal sphincter. Fourth Degree: Sphincter torn, anal mucosa involved. Central Tear: Head penetrates posterior vaginal wall, then perineal body. Management: First-degree: Not sutured unless extends to perineal skin. Second-degree: Always sutured carefully. Third/Fourth-degree: Surgical emergency, repaired immediately under anesthesia. Meticulous suturing of rectal wall, perineal body muscles, external sphincter. Aftercare: Keep wound clean, frequent swabbing, antiseptic solution, antibiotics, bowel confinement (5 days), stool softeners. Overlap technique for sphincter repair (controversial). Old, Longstanding Complete Perineal Tears Appearance: Red mucous membrane of anal canal/rectum protrudes, no perineal tissue. Depression at severed sphincter ends. Symptoms: Incontinence of faeces and flatus. Diagnosis: Clinical exam, perineal ultrasound, MRI. Treatment: Operative, 3-6 months post-delivery. Preoperative bowel preparation (aperients, enemas, antibiotics, non-residual diet). Dissection of rectum from vagina, mobilization, repair of anal canal/rectum, suturing of perineal body and external sphincter. Aftercare: Keep wound dry, antiseptic, powdered. Bowel confinement (5 days), IV/oral fluids, small laxative. Foley's catheter. Systemic antibiotics. Vaginal Tears Isolated, often instrumental/manipulative delivery. Prompt repair to prevent blood loss. May use vaginal packing. Cervical Tears Instrumental delivery, shoulder dystocia, breech delivery. Suspect with excessive vaginal bleeding despite well-contracted uterus. Speculum exam and ring forceps inspection for repair. Colporrhexis Rupture of vaginal vault. May have concomitant cervical tear. Extensive injury may lead to broad ligament haematoma, requiring laparotomy. Suturing of rent. Care to avoid uterine vessels and ureter. Injuries Due to Coitus Defloration: Slight bleeding common, severe hemorrhage rare (vestibule tear). Early Marriage: Bruising of vaginal wall, urethritis ("honeymoon cystitis," pyelonephritis). Lacerations: Violent coitus/rape (young girls), forceful penetration (postmenopausal, atrophy, malformations). Longitudinal tear of anterior vaginal wall common. Posterior vaginal wall rupture can open peritoneal cavity. Bladder/rectum involvement. Post-Op: After vaginal operations or total hysterectomy, coitus too soon can disrupt healing. Spontaneous Rupture: In upper posterior one-third of vagina, in elderly atrophic women, due to violent coughing/straining. Management: Small injuries: vaginal plugging. Severe: suturing under anesthesia. Prolapsed bowel: laparotomy, bowel inspection/repair. Direct Trauma and Vulval Haematoma Causes: Falls (astride gates/chairs), inadequate hemostasis during episiotomy/perineal tear repair. Haematoma: Large haematomas in labia majora (clitoris/erectile tissue involvement), rupture of varicose veins (pregnancy). Symptoms: Painful tender swelling (bluish-black), pallor, shock. Management: Small: bed rest, sitz bath, magnesium sulphate fomentation, antibiotics. Large: incise, remove clot, secure hemostasis, packing/drainage. Deep penetrating injuries: immediate surgery. Suspected visceral injury: laparotomy. Pelvic Haematoma Infralevator Haematoma: Following perineal tear/episiotomy. Supralevator Haematoma (Broad Ligament): Following cervical tear (uterine vessels), uterine rupture, uterine artery tear during surgery. Symptoms: Hypotension, tachycardia, pallor, tender swelling beside uterus. Management: Small: conservative (observation, antibiotics). Large: laparotomy (packing, blood transfusion), hysterectomy (uterine rupture), internal iliac ligation, embolization. Genital Mutilation Partial/total removal of external genital organs for non-medical reasons (Africa, Asia, Arabs). Types: Type I (clitoris/prepuce), Type II (clitoris/labia minora), Type III (clitoris/labia minora, apposing), Type IV (pricking, piercing, incision, cauterization). Immediate Complications: Bleeding, pain, infection. Long-term Complications: Chronic pain, dyspareunia, apareunia, haematoma, scarring, HIV/tetanus, retention of urine, haematocolpos, difficult childbirth, psychological trauma. Injuries Due to Foreign Bodies and Instruments Vagina: Foreign bodies: Pins, hair grips, pencils, jars (mentally retarded, young children). Present with persistent, malodorous discharge. Neglected therapeutic objects: Ring pessary (ulceration, carcinoma). Forgotten swabs/tampons (foul discharge). Contraceptive devices: Cervical caps, diaphragms, condoms (discharge, ulceration). Instrumental damage: During criminal abortion (sound, gum, needles). Perforation into bladder, rectum, pouch of Douglas. Treatment: Removal of foreign body. Antibiotics for perforation. Laparotomy for peritonitis/bowel damage. Cervix: Obstetric tears: Precipitate labor, instrumental delivery. Iatrogenic tears: Cervical dilation (bleeding, incompetent os). Conization/amputation/cauterization (stenosis, haematometra, infertility). Uterus: Intrauterine contraceptive devices (IUCDs): Neglected, forgotten. Ulceration, ascending infection, meno-rrhagia. Perforation into myometrium or peritoneal cavity. Abortion attempts: Serious intrauterine infections, pelvic abscess. Perforation: During D&C, MTP, hysteroscopic procedures (TCRE, septum division). Risk of injury to viscera/vessels. Asherman syndrome: Vigorous curettage, uterine packing, manual placenta removal, infection. Treatment: Remove foreign bodies. Antibiotics for infection. Laparotomy for adnexal involvement or perforation with prolapsed intestine. Repair of rent (if uterus contains products of conception). Hysterectomy for large perforation/completed family. Chemical and Other Burns of the Vagina Causes: Strong chemicals (lysol, permanganate, corrosive sublimate) for abortion. High-temperature douches. Cauterization of cervix (direct or conduction burn). Laser therapy. Radiation (radium for cervical carcinoma). Complications: Extensive vaginal adhesions, fibrosis, obliteration of canal, dyspareunia, menstrual retention, haematometra, pyometra. Radiation burn leads to adhesive vaginitis, fibrosis. Treatment: Expectant for mild burns. Plastic surgery for severe scarring/atresia. Injuries of the Intestinal Tract Close anatomical relation to lower female genital tract. Risk during vaginal delivery, vaginal surgery, abdominal gynaecological surgery. Cautery can cause delayed GIT burns. Bowel Injuries in Obstetrics and Gynaecology Vaginal Delivery: Third- and fourth-degree perineal tear. Rectovaginal fistula. Faecal incontinence. Stricture of anal canal/rectum. Caesarean Delivery: Intestinal injury. During MTP. Other Causes: Congenital rectovaginal fistula, penetrating injury, infections (STIs, septic abortions), rectal/pelvic abscess. During Surgery: Abdominal hysterectomy, vaginal surgery (posterior repair, vaginoplasty), endoscopic (laparoscopy, hysteroscopy). Genital Cancers. Radiotherapy. Vaginal Delivery and Bowel Injury Injury to anal sphincter, anal canal, rectum common in primiparae. Risk Factors: Big baby, prolonged labor, occipitoposterior presentation, breech, forceps delivery, rigid perineum, midline episiotomy. Injury can be direct muscle trauma, pelvic floor muscle injury, or pudendal nerve injury. Symptoms: Immediate or delayed (anal wall prolapse, faecal incontinence). Faecal Incontinence Definition: Involuntary leakage of faecal contents. Normal Continence: Internal sphincter (autonomic), external sphincter (striated, pudendal nerve), puborectalis muscle. Anal pressure > rectal pressure. Rectum-anal canal angle (60-130°). Aetiology: Obstetric Trauma: Prolonged labor (overstretching levator ani, pudendal nerve damage), difficult forceps, occipitoposterior, big baby, rigid perineum, midline episiotomy, 3rd/4th-degree tears. Non-Obstetric: Neurogenic (dementia, CVA, MS), bowel diseases (IBD, cancer, prolapse), radiotherapy. Symptoms: Leakage of flatus, loose motion, or solid stool. Reluctance to disclose. Investigations: Proctoscopy, sigmoidoscopy, manometry, electromyography (EMG), transrectal ultrasound, MRI. Treatment: Medical: Loperamide, codeine phosphate, fibre-rich diet, antidiarrhoeal. Physiotherapy: Pelvic floor exercises, biofeedback. Sacral nerve stimulation. Surgery: For extensive tears, fistula, anal prolapse (rectopexy). Elective caesarean section for future pregnancies. Rectovaginal Fistula Causes: Obstetric: Incompletely sutured complete perineal tear. Iatrogenic: Post-perineorrhaphy (thin, elderly patients), pelvic abscess drainage through posterior fornix. Infective: Tuberculosis, lymphogranuloma inguinale, anal crypt infection. Malignancy: Advanced cervical carcinoma, radiation treatment, primary rectal carcinoma. Congenital. Rare: Diverticulitis, rectal abscess, direct trauma. Symptoms: Incontinence of faeces and flatus. Diagnosis: Visual inspection (large), proctoscopy, sigmoidoscopy, radiopaque dye injection. Treatment: Operative: Preoperative bowel prep (enema, antiseptics, antibiotics). Small fistula: Excision of tract, local closure. Large fistula with inadequate perineal body: Cut skin bridge to convert to complete perineal tear, then repair. High fistula: Preliminary colostomy. Malignant/radiation fistula: Exenteration or colpocleisis (obliteration of vaginal cavity, poor results). Bowel Injury (General) Aetiology: Entering Peritoneal Cavity: Obesity, previous surgery, pelvic endometriosis, PID, cancer surgery, previous irradiation. Laparoscopy: Veress needle/trocar perforation, cautery/laser burns (delayed presentation). Hysteroscopy: Uterine perforation (TCRE, septum resection), thermal heat. D&C: Rare. Caesarean Section: Small bowel injury (adherent intestine). MTP: Uterine perforation with bowel loop pulled through. Criminal Abortion. Infections: STIs (condyloma venereum stricture). Types: Perforation, laceration, crush injuries. Diagnosis: Most recognized at surgery. Burns present after 5-7 days as peritonitis/fistula. Surgical Treatment: Small injury ( Larger laceration: Resection and end-to-end anastomosis. Colonic injury: Proximal colostomy. Rectal injury: Suturing (small tear), proximal colostomy (large hole). Prevention: Proper obstetric management. Identify high-risk factors in gynaecological surgery. Sharp dissection for endometriosis/PID. Careful use of cautery/laser in laparoscopy.