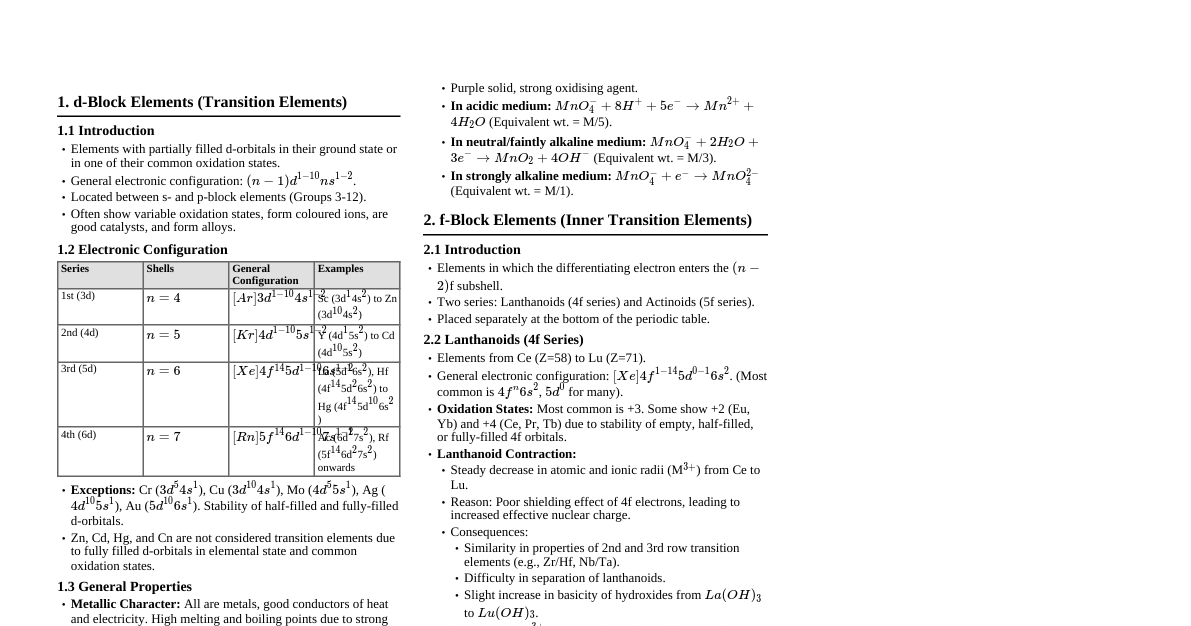
The Discharging Ear Introduction Otorrhea: Common complaint in otorhinolaryngology. Ear discharge can be wax or from external/middle ear diseases. Clear discharge could be cerebrospinal fluid (CSF) otorrhea. Causes of Ear Discharge Otitis externa Granular myringitis Acute otitis media (AOM) Chronic otitis media (COM): Mucosal or squamous type Tuberculous otitis media Postmastoidectomy cavity External or middle ear neoplasms Foreign body in the ear canal CSF otorrhea Evaluation of a Patient Presenting with Ear Discharge Detailed history: Type, mode of onset, duration, associated complaints. External ear infections: Purulent ear discharge, often with ear pain. Middle ear infections: Mucoid or mucopurulent ear discharge. AOM: Preceding upper respiratory tract infection, ear block, ear pain reducing with discharge onset. Mucosal COM (tubotympanic): Profuse, intermittent mucopurulent discharge, aggravated by upper respiratory infections. Squamous COM (atticoantral): Foul-smelling, scanty, purulent, continuous discharge; blood-stained if granulation tissue present. Blood-stained discharge: Tumors of external/middle ear, trauma. Enquire about hearing loss, tinnitus, vertigo. Vertigo: Complications like labyrinthitis or labyrinthine fistula. Facial palsy with otorrhea: Complication of AOM, cholesteatoma, malignant otitis externa, temporal bone trauma, tuberculous otitis media, herpes zoster oticus (Ramsay Hunt syndrome). Petrositis: Deep-seated retro-orbital pain, diplopia. CSF leak: History of head injury or mastoid surgery, watery discharge. Examination of the Ear Tragal tenderness: Otitis externa. Mastoid tenderness: Acute mastoiditis. Otoscopic (otoendoscopic/microscopic) examination: Identifies cause based on external auditory canal and tympanic membrane features. Otitis externa: Inflamed and swollen external auditory canal, otomycotic debris. Malignant otitis externa: Granulation tissue in floor of external auditory canal at bony-cartilaginous junction. AOM: Perforation in anteroinferior quadrant with pulsatile ear discharge; congested pars tensa. Acute mastoiditis: Sagging of posterosuperior canal wall. Mucosal COM: Central perforation (perforation of pars tensa with margins formed by remnants of pars tensa). Squamous COM: Marginal, total, or attic perforation; retraction pocket in posterosuperior quadrant or attic with cholesteatoma. Post-mastoidectomy cavity (post-MRM) recurrent/persistent discharge: Recurrent or residual disease. Large cavity. Deep recess at mastoid tip. High facial ridge. Inadequate saucerization of cavity. Inadequate meatoplasty. Exposed eustachian tube area. Ulceration and granulation, or mucosalization of cavity lining. Tuberculous otitis media: Multiple perforations coalescing into large perforation; pale granulations in middle ear. Investigations Otomicroscopy/otoendoscopy: Confirms diagnosis; swab for culture/antibiotic sensitivity; ear discharge cleaned. Audiometry: Documents type and degree of hearing loss. Radiological investigations: HRCT scan: Temporal bone trauma, malignant otitis externa. Contrast-enhanced CT scan or MRI: Complications of otitis media or neoplastic lesions. Biopsy: Lesion in external auditory canal or middle ear not responding to medication (after imaging). Treatment of Ear Discharge Directed at treating underlying cause and preventing complications. Otitis Media Introduction Inflammation or infection of the middle ear space. Spectrum of diseases: AOM, COM, otitis media with effusion (OME). Most inflammatory diseases related to eustachian tube dysfunction. Classified as suppurative or nonsuppurative based on pus formation. Nonsuppurative otitis media: Inflammatory, no suppuration. Includes: Eustachian tube dysfunction (ETD) OME Atelectasis Adhesive otitis media Tympanosclerosis Otitic barotrauma (aerotitis) Otitis Media with Effusion Synonyms: Secretory otitis media, serous otitis media, seromucinous otitis media, glue ear. Definition: Effusion in middle ear space without signs/symptoms of acute ear infection. Characteristics: Nonpurulent fluid (thick/viscid like glue, common in children 2-5 years; thin/watery/serous, usually in adults). Etiology Eustachian Tube Dysfunction (ETD) Affects ventilation and drainage of middle ear. Conditions causing ETD: Congenital palatal abnormalities (e.g., cleft palate) Syndromic children with craniofacial anomalies and trisomy 21 Infections of nose, paranasal sinuses, nasopharynx, adenoids Ciliary dysfunction (Kartagener's syndrome, smoking) Surfactant deficiency Benign and malignant tumors of nose, paranasal sinuses, nasopharynx Trauma Allergy Hormonal factors (high estrogen, hypothyroidism) Palatal paralysis Postradiotherapy Unresolved Acute Otitis Media (in Children) Impaired middle ear drainage + low-grade infection $\rightarrow$ stimulates middle ear mucosa to secrete more fluid. Bacterial Biofilms Possible cause for middle ear effusion with ETD as a secondary factor. Other Predisposing Factors Parental smoking Daycare attendance Pearl Nasopharyngeal tumor should be suspected in adult patients with unilateral OME. Clinical Features Symptoms No symptoms, or hearing loss with seasonal fluctuation. Children with OME: Conductive hearing loss (usually More adversely affected: Craniofacial anomalies, syndromes, autism, blindness. Prior history of repeated upper respiratory infections with otalgia, followed by reduced hearing. Adults: Ear block, tinnitus, decreased hearing, autophony; occasionally vertigo. Signs Otoscopic (otoendoscopic/microscopic) examination: Opaque with amber or gray colored tympanic membrane. Distorted or absent cone of light. Foreshortened handle of the malleus. Mild to severe retraction of tympanic membrane with prominent (sickle-shaped) anterior and posterior malleolar folds. Reduced or absent mobility of tympanic membrane on air insufflation (Valsalva's maneuver or Siegelization). Air-fluid level or bubbles of air. Pneumatic otoscopy: Routinely done to aid diagnosis; notes movement of tympanic membrane during compressed bulb release. Pearl Signs of a retracted tympanic membrane: Dull, lusterless tympanic membrane. Absent or distorted cone of light. Apparent foreshortening of the handle of the malleus. Prominent lateral process of the malleus. Prominent anterior and posterior malleolar folds (sickle shaped). Reduced mobility of the tympanic membrane on Valsalva's maneuver, Toynbee's maneuver, or Siegelization. Table 8.1 Grades of retractions of the tympanic membrane Grade Pars tensa (Sade) Pars flaccida (Tos and Paulsen) 1 Slight retraction of tympanic membrane over its annular fold Small attic dimple 2 Severe retraction of the tympanic membrane. It is draped over the long process of incus and incudostapedial joint Pars flaccida is retracted and in contact with the neck of the malleus 3 Atelectasis: the tympanic membrane is in contact with the promontory but is mobile with Valsalva's maneuver Here in addition to grade 2 features, there is minimal erosion of the outer attic wall 4 Adhesive otitis: the tympanic membrane is adherent or stuck to the promontory. It does not move with Valsalva's maneuver Deep retraction with severe erosion of the outer attic wall Investigations Tuning fork tests: Mild to moderate conductive hearing loss (difficult in younger children). Pure tone audiometry (PTA): Mild-to-moderate conductive hearing loss. Tympanometry: Flat tympanogram ("B" type) due to reduced tympanic membrane compliance. Reliable in infants >4 months. Important for documentation. Tests for speech delays. Children: Nasopharynx evaluated for adenoid hypertrophy (X-ray lateral view). Adults: Diagnostic nasal endoscopy to rule out nasopharyngeal lesion. Treatment Observation: If OME Antibiotics: Erythromycin, co-trimoxazole, co-amoxiclav controversial. Recent studies show metabolically active bacteria in culture-negative effusions; antibiotics may have short-term benefits. Nasal decongestants and antihistamines: Limited success. Corticosteroids: Short course in adults for resistant cases (effectiveness uncertain). Exercises: Valsalva's maneuver, Toynbee's maneuver, politzerization, Otovent autoinflation device (for children >3 years) to ventilate middle ear. Avoid during upper respiratory tract infection. Surgery: Restores middle ear ventilation by eliminating infection source/ETD cause, drains middle ear effusion. Myringotomy and grommet insertion: Common procedure. Aspiration of middle ear fluid via radial incision in anteroinferior quadrant of tympanic membrane. Grommet (ventilation tube) inserted for middle ear ventilation. Adenoidectomy: Removes nasopharyngeal obstruction to eustachian tube and infection focus in adenoids. Eustachian tuboplasty: Laser, microdebrider, balloon dilatation for persistent/recurrent OME to improve dilatory function (good results, long-term assessment needed). Steroids: Treatment for OME controversial. Topical steroid nasal sprays (mometasone) prescribed, but clear evidence of effectiveness lacking. Otitic Barotrauma Synonyms: Aerotitis media, barotitis media. Condition from ETD failure to maintain middle ear pressure at ambient atmospheric level. Symptoms manifest during deep sea/scuba diving or descent from altitude during air travel. Changes can occur under less marked ambient pressure fluctuation. Incidence higher in nonpressurized aircrafts. Predisposing Factors Poor eustachian tube function. Recent upper respiratory tract infection. Sleeping during flight or during descent (cannot equalize pressure). Deviated nasal septum (cannot equalize pressure). Clinical Features Patient complaints: Aural fullness, popping sensation, discomfort, pain. Typically asymptomatic once returned to ground level. Significant barotrauma: Temporary middle ear effusion or hemotympanum. Occurs when atmospheric pressure > middle ear pressure by 90 mmHg; ET locks, negative pressure $\rightarrow$ tympanic membrane retraction, transudation/hemorrhage. Rapid pressure change: Tympanic membrane rupture. Change in pressure: Can affect inner ear $\rightarrow$ sensorineural hearing loss (SNHL) and vertigo (bleed in inner ear, intralabyrinthine membrane rupture). Diagnosis: By history. PTA: Conductive hearing loss; rarely SNHL or mixed hearing loss. Treatment Mainly symptomatic with decongestants and analgesics. Topical nasal decongestants: Xylometazoline or oxymetazoline (open ET). Oral decongestants: Phenylephrine. Eustachian tuboplasty: Helpful for frequent flyers. Long-standing ventilation tube: Useful in professional/frequent flyers. Prevention Avoid traveling during upper respiratory tract infection. Correction of deviated nasal septum. Oral or topical nasal decongestants prior to travel. Acute Otitis Media Introduction Acute infection of middle ear mucoperiosteum by pyogenic organisms. One of the commonest infections in preschool children. Prevalence in India: 17-20%. Common during winter months, in non-breastfed children. Recurrent AOM: >3 episodes in 6 months or 4-6 episodes in 1 year. Resistant AOM: Persists despite 3-5 days of antibiotics. Predisposing Factors Age: 6 months to 3 years. Allergies and genetic factors. Bottle feeding at early age (supine position) and pacifier use. Craniofacial anomalies: Cleft palate, Down's syndrome. Crowded living conditions, low socioeconomic status. Cystic fibrosis and primary ciliary dyskinesia. Anemia. Immunoglobulin deficiency (IgG, IgM). Exposure to smoke. Exposure to viral infections in day-care centers. Gastroesophageal reflux. Immunodeficiency. Etiopathogenesis Viral upper respiratory tract infection $\rightarrow$ middle ear via ET $\rightarrow$ inflammatory mediators, reduced ciliated cells, increased mucous production. Increased fluid + impaired drainage $\rightarrow$ secondary bacterial infection. Children: Immature immune system. Infants: ET wider, shorter, more horizontal $\rightarrow$ prone to AOM. Bottle-fed in supine position $\rightarrow$ milk into ET. Infections (adenoiditis, tonsillitis, pharyngitis, rhinosinusitis) $\rightarrow$ middle ear via ET. Forceful nose blowing/Valsalva's maneuver + rhinitis $\rightarrow$ infection into ET. Deep sea diving, barotrauma, swimming $\rightarrow$ AOM. Unpressurized aircraft + rhinitis $\rightarrow$ AOM. Traumatic perforations $\rightarrow$ infection spread into middle ear via external ear. Middle ear infection rarely blood borne. Causative Organisms Common: $S$. pneumoniae, $M$. catarrhalis, $H$. influenza. Other: $S$. aureus, $S$. haemolyticus. Rarely: Gram-negative bacilli (Proteus, $E$. coli). Clinical Features Usually preceded by viral upper respiratory tract infection. Rapid onset of ear pain, more severe at night. Infants: Irritability, intense crying, poor feeding. Toddlers: Clutch/rub ear, cry, sleep affected. Clinical features described in five stages. Table 8.2 Five stages based on the course of the disease Stage Symptoms Signs Stage of tubal occlusion (catarrhal stage): Eustachian tube obstruction resulting from inflammatory edema in the nasopharynx causes absorption of oxygen and increase in carbon dioxide in the middle ear Blocking sensation/fullness in the ear Mild ear pain Mild deafness Fever and malaise Retracted tympanic membrane with loss of light reflex Tuning fork tests show conductive hearing loss Stage of presuppuration: Persistent occlusion of the eustachian tube causes exudation from capillaries in the middle ear due to mucosal congestion Severe throbbing type of ear pain, which worsens during sleep because of venous congestion in the recumbent position Tinnitus, i.e., bubbling sounds are heard Deafness, which goes unnoticed due to the severity of pain Fever and malaise. The patient looks toxic Congested tympanic membrane with prominent blood vessels in the pars tensa giving it a cartwheel appearance Congestion of the pars flaccida due to epitympanitis Tuning fork tests show a conductive hearing loss Stage of suppuration: There is accumulation of pus in the middle ear. Tympanic membrane bulges laterally due to pus under tension Excruciating ear pain Deafness Fever and other constitutional symptoms Congested and bulged tympanic membrane with loss of landmarks A yellow nipple is seen on one spot of the tympanic membrane suggesting impending rupture Tenderness over the suprameatal triangle due to mastoiditis Stage of resolution: The tympanic membrane ruptures at its weakest part causing otorrhea while other symptoms begin to abate Blood-stained mucopurulent ear discharge Fever, ear pain, and constitutional symptoms subside Perforation in the anteroinferior quadrant of the pars tensa with blood-stained mucopurulent ear discharge coming out under pressure, which may be pulsatile. This is also known as the light house sign Conductive hearing loss Stage of Complications Untreated/inadequately treated inflammation $\rightarrow$ complications (reduced host immunity, high organism virulence). Infection spread to mastoid air cell system $\rightarrow$ acute mastoiditis, abscess. Other complications: Labyrinthitis, petrositis, facial paralysis, lateral sinus thrombophlebitis, meningitis, extradural abscess, brain abscess. Pearl Excessive crying in children can lead to tympanic membrane congestion, but it is not edematous and light reflex is present (differentiates from AOM). Management Diagnosis is clinical. Ear discharge sent for culture and sensitivity. Investigations (CT/MRI temporal bone/head) only for suspected complications or failure to improve with medications. Complete blood picture, C-reactive protein, blood culture for severe complications. Treatment Relief from symptom. Control and eradicate middle ear infection. Ensure ET patency for middle ear ventilation and drainage. Return of auditory function. Prevention Vaccination (H. influenza, Pneumococcus, Influenza A virus) reduces AOM incidence and severity. Breastfeeding infants up to 6 months is protective. Medical Treatment Catarrhal stage: Antibiotics usually not required, most cases resolve spontaneously. Topical (nasal) decongestants: Oxymetazoline (0.025% children, 0.05% adults), xylometazoline (0.05% children, 0.1% adults). Oral decongestants: With or without antihistamines. Help relieve mucosal edema around ET, improving middle ear ventilation. Note: Some studies conclude decongestants/antihistamines don't play a role, but can reduce nasal symptoms in preexisting rhinitis. Antibiotics: Started at earliest suspicion of suppuration. Amoxicillin 40 mg/kg/d in 3 divided doses for 7-10 days. Amoxicillin with clavulanate, cefixime, or cefuroxime for beta-lactamase producing organisms. Oral cephalosporins (cefdinir, cefuroxime, cefpodoxime) or macrolides (clarithromycin) for penicillin allergy. Parenteral antibiotics (amoxicillin with clavulanate or ceftriaxone) for 24-48 hours, followed by oral for 7 days, for severe infection. Topical antibiotic ear drops: Not given with discharge or pinhole/small perforation (may not enter middle ear). Aural toilet: Removes discharge. Analgesics and antipyretics: Ibuprofen and/or acetaminophen for pain and fever. Surgical Treatment Resorted to when medical management fails or impending complications. Three types: Diagnostic, therapeutic, prophylactic. Tympanocentesis: Diagnostic procedure, aspirates middle ear fluid with needle. Aspirate sent for culture/sensitivity. Relieves pressure, reduces pain. Myringotomy: Therapeutic procedure, curvilinear incision in posteroinferior quadrant of tympanic membrane for drainage and ventilation. Performed in exudative stage (bulging tympanic membrane with pus). Suppurative stage (small perforation, inadequate drainage). AOM with impending complications. Myringotomy and grommet insertion for recurrent AOM. Sequelae of Acute Otitis Media Conductive hearing loss due to failure of resolution. Sensorineural hearing loss due to inner ear damage (toxins absorbed via round window membrane). Persistent perforation due to ET pathology (common with large kidney-shaped perforation or poorly pneumatized mastoid). Atelectasis of tympanic membrane due to persistent ET pathology. Healing of perforation with scarring of tympanic membrane or tympanosclerosis. Healing with dimeric membrane formation at perforation site (middle fibrous layer absent). Pearl Most central perforations of tympanic membrane (pars tensa) are kidney shaped (avascular region between handle of malleus and peripheral annular region with abundant blood supply). Acute Necrotizing Otitis Media Severe, virulent form of AOM with necrosis of tympanic cavity. Common in pre-antibiotic era, less common now. Rapid onset/progression. Seen in children with influenza, typhoid, measles, scarlet fever. Immunocompromised/malnourished children at higher risk. Due to secondary infection by $\beta$-hemolytic streptococci, causing necrosis of tympanic membrane (annulus, ossicular chain, middle ear mucosa, mastoid air cells). Characterized by profuse otorrhea, kidney-shaped or near-total perforation, moderate to severe hearing loss (conductive or mixed). Treatment: Early antibiotics (10-14 days). Cortical mastoidectomy if medical treatment fails or complicated by acute mastoiditis. Healing leads to tympanic membrane fibrosis or squamous epithelium ingrowth from external auditory meatus. Chronic Otitis Media (Chronic Suppurative Otitis Media) Types of Chronic Otitis Media Traditionally classified as: Mucosal type or tubotympanic disease (TTD). Squamous type or atticoantral disease (AAD). Mucosal Type or Tubotympanic Disease (TTD) Mainly involves anteroinferior part of middle ear cleft. Associated with pars tensa perforation and ear discharge. Perforation is "central" (in pars tensa, surrounded by pars tensa remnant). Ear discharge usually mucoid (goblet cells in anteroinferior middle ear cleft); can be mucopurulent. Can be active or inactive. Active Disease Pars tensa perforation + ear discharge and/or middle ear inflammation, granulation tissue, polyps. Discharge present at examination. Inactive Disease Pars tensa perforation + absence of ear discharge and/or middle ear inflammation or polyps. No discharge at examination. Note: In previous nomenclature (CSOM-tubotympanic type), four stages: Active stage: Discharge and/or congested middle ear mucosa, granulation, or polyp. Quiescent stage: Perforation, no discharge, last discharge within 6 months. Inactive stage: Perforation, last discharge >6 months ago. Healed stage: Dry (non-discharging) ears, tympanic membrane perforation heals itself in two layers (dime ric membrane without middle fibrous layer); may be associated with tympanosclerosis, conductive hearing loss. Permanent perforation: In long-standing infections, squamous epithelium lines perforation edges ("contact inhibition"); insufficient blood supply, connective tissue hyperproliferation, less growth factors at margins. Squamous Type or Atticoantral Disease (AAD) Chronic inflammatory condition of middle ear cleft, usually involving posterosuperior part of mesotympanum, attic, antrum. Associated with entrapment of keratinizing squamous epithelium (cholesteatoma) in middle ear space. Cholesteatoma can erode and destroy adjacent temporal bone tissues. Also called AAD or "unsafe type" of CSOM (due to site of involvement, potential for intra- and intracranial complications). Squamous CSOM has two stages: Active: Cholesteatoma and granulation tissue present. Inactive: Retraction pocket, no cholesteatoma or granulation tissue. Cholesteatoma Synonyms: Epidermosis, keratoma. Term "cholesteatoma" coined by Johannes Mueller in 1838. Misnomer (not a tumor, no cholesterol). Also "skin in the wrong place." Sac lined by stratified squamous epithelium with central mass of keratin debris. Bone-eroding properties. Consists of two parts: Matrix: Squamous epithelium (stratum basale, superficiale, corneum) resting on thin fibrous stroma (perimatrix). Central white mass: Keratin debris produced by matrix. Causes of bone destruction: Hyperemic decalcification. Osteoclastic bone resorption (enzymes: acid phosphatase, collagenase, acid proteases, proteolytic enzymes, leukotrienes, cytokines). Pressure necrosis. Flowchart 8.1 Types of Cholesteatoma Congenital Acquired Primary Secondary Tertiary Congenital Cholesteatoma Originates from embryonal inclusion of squamous epithelium (cell rests) in middle ear cleft or temporal bone. Usual sites of epithelial cell rests: Tympanic cavity, petrous apex, cerebellopontine angle. Presents as a white mass behind an intact tympanic membrane with conductive hearing loss. Diagnostic criteria: Intact tympanic membrane. No previous history of otitis media. Acquired Cholesteatoma Primary acquired cholesteatoma: Formed in attic (pars flaccida) or posterosuperior quadrant (pars tensa) retraction pocket. Little/no history of ear discharge. Secondary acquired cholesteatoma: Occurs in marginal perforation (posterosuperior quadrant of pars tensa) or long-standing pars tensa perforation with epithelium growth from margins onto medial middle ear wall. Foul-smelling ear discharge, granulation tissue, polyps. Tertiary acquired cholesteatoma: Following trauma or tympanoplasty (graft cholesteatoma after onlay myringoplasty). Pathogenesis of Acquired Cholesteatoma ETD $\rightarrow$ middle ear pressure fluctuations. Blocked ET $\rightarrow$ air absorbed $\rightarrow$ negative middle ear pressure $\rightarrow$ retraction of pars flaccida and pars tensa. Theories of Cholesteatoma Formation Invagination or Retraction Pocket Theory (Wittmack) Primary mechanism: Retraction pocket in attic or posterosuperior quadrant of pars tensa with erosion of adjacent canal wall. ETD and/or epitympanic dysventilation $\rightarrow$ retraction. Pocket deepens due to negative middle ear pressure and repeated inflammation. Sac loses self-cleansing, secondary infection of keratin matrix. Sac expands $\rightarrow$ attic perforation or medial progression. Epithelial Invasion/Migration Theory (Habermann) Keratinizing squamous epithelium from surface of tympanic membrane or external auditory canal migrates into middle ear through preexisting perforation. Epithelial cells migrate by "contact guidance." Stop migrating when encountering another epithelial surface ("contact inhibition"). Basal Cell Hyperplasia (Ruedi and Lange) Inflammatory stimulus $\rightarrow$ basal cells of stratum corneum from keratinizing epithelium of pars flaccida invade subepithelial space $\rightarrow$ attic cholesteatoma. Metaplasia (Wendt) Pluripotent middle ear epithelium stimulated by inflammation $\rightarrow$ metaplastic stratified squamous epithelium with keratinization. Implantation Theory Iatrogenic implantation of skin into middle ear (tympanoplasty). Rare complication of myringotomy and grommet insertion. Epithelium entrapment through fracture line following trauma. Expansion of Cholesteatoma Enters middle ear cleft, invades surrounding structures by path of least resistance, then enzymatic bone destruction. Pars flaccida cholesteatoma: Originates in Prussak's space (below scutum, limited by tympanic membrane, malleus neck, lateral malleus ligament) $\rightarrow$ laterally toward ossicular chain and into epitympanum. Pars tensa cholesteatoma: Begins posterosuperiorly $\rightarrow$ posteriorly toward facial recess and tympanic sinus, medially toward ossicular chain. Clinical Features Symptoms Persistent, scanty, purulent, foul-smelling, painless ear discharge. Blood-stained discharge with granulations or polyps. No relation of discharge to upper respiratory tract infection; usually doesn't completely subside with medication. Hearing loss: Usually conductive. Normal in limited pars flaccida disease. Cholesteatoma hearer: Ossicular chain erosion, but gap bridged by cholesteatoma mass, so hearing is normal. Progressive hearing loss: Conductive (ossicular involvement) or mixed (conductive and sensory) if inner ear involved (bacterial toxins, ototoxic drugs, cochlea/lateral semicircular canal erosion). Ear pain: Otitis externa secondary to discharge irritation. Dull pain from cholesteatoma filling mastoid antrum. Tinnitus and giddiness. Symptoms associated with complications: Sudden severe vertigo (disease eroding into lateral semicircular canal). Sudden severe deafness (disease eroding into cochlea). Paralyzed face (disease affecting facial nerve). Swelling around ear with pain (mastoiditis). Fever, neck stiffness, severe headache (meningitis). Headache, retro-orbital pain, diplopia (petrositis). Headache, blurred vision, projectile vomiting (intracranial complications). Signs Retraction pocket or invagination of tympanic membrane in attic or posterosuperior pars tensa (squamous—inactive). Perforation seen in attic (pars flaccida) or posterosuperior quadrant of pars tensa with marginal involvement. Attic perforation may be hidden by dried discharge/crusts. Attic disease can erode lateral attic wall $\rightarrow$ auto-atticotomy cavity. Posterior extension into antrum $\rightarrow$ auto-mastoidectomy cavity. Crusts over pars flaccida should be removed. Even with pars tensa (central) perforation, examine pars flaccida for double pathology (squamous disease takes precedence). Total perforation involves fibrous annulus. Cholesteatoma debris or flakes in retraction pocket and other middle ear cleft parts. Granulation tissue in pars flaccida, posterosuperior pars tensa, or posterosuperior deep meatus. During mastoidectomy, granulation in middle ear and mastoid. Perforation in pars tensa with ingrowing epithelium (posterior margin), spreading onto medial tympanic cavity wall (velvety appearance). Aural polyp filling external auditory meatus. Types of Perforations of the Tympanic Membrane Tympanic membrane (pars tensa, pars flaccida). Pars tensa divided into four quadrants (anterosuperior, anteroinferior, posterosuperior, posteroinferior) by vertical line along malleus handle and horizontal line at umbo. Characterized by site, type, and annulus involvement. Perforation of Pars Tensa Central Perforation: Perforation of pars tensa, margins formed by remnants of pars tensa. "Safe perforation." Small: One quadrant or Medium: Two quadrants or 10-40% pars tensa. Large: Three or more quadrants or >40% pars tensa. Subtotal: All four quadrants, reaches fibrous annulus but not involving it. Malleus handle may be skeletonized. Marginal Perforation: Perforation in pars tensa (commonly posterosuperior quadrant) that erodes annulus and one margin (sulcus tympanicus). "Unsafe perforation." Total Perforation: Complete perforation of pars tensa, margins formed by bony annulus. "Unsafe perforation." Traumatic Perforation Usually in posteroinferior quadrant, ragged edges with blood clots. Causes: Slap on ear, sharp foreign body, iatrogenic/blast injury. Perforation of the Pars Flaccida Attic Perforation: Seen in pars flaccida. Associated with cholesteatoma. "Unsafe perforation." Seen in squamous COM or AAD. Traumatic Tympanic Membrane Perforation Causes: Slap on ear, blast injury, attempted self-cleaning, pressure changes, iatrogenic injury (wax/foreign body removal, syringing, instrumentation). Clinical Features Pain, bleeding from ear, tinnitus (usually subsides). Vertigo may be present. Ossicular chain (conductive) and inner ear (sensorineural) involvement depends on type/intensity of trauma, affecting hearing. Examination: Commonly posteroinferior pars tensa perforation (due to external auditory canal curvature). Ragged edges with blood clots. Recent trauma may show blood in canal/over perforation. Tuning fork tests help initial hearing assessment. Treatment Reassurance, wait-and-watch, regular follow-up. PTA to document hearing (medicolegal cases). Aural hygiene (prevent water entry, avoid earbuds). Margins may be brought together under microscope. Topical ear drops not used. Contaminated injuries: Cleaning under microscope, oral antibiotics. Most traumatic perforations heal spontaneously. If perforation persists, myringoplasty. Chronic Otitis Media–Mucosal Type or Chronic Suppurative Otitis Media–TTD Definition Chronic inflammatory condition of middle ear cleft (ET, tympanic cavity, aditus, antrum, mastoid air cells). Characterized by permanent pars tensa perforation with/without intermittent otorrhea and hearing loss. Also known as: CSOM-tubotympanic type (disease mainly involves anteroinferior middle ear cleft/tympanic cavity adjacent to ET). Safe ear or benign type of CSOM (inflammation leads to profuse discharge from mucous glands/goblet cells, no important structures involved, less complications). Pearl Central perforation of pars tensa is hallmark of mucosal COM. Epidemiology Common cause of conductive hearing loss, especially in rural population (lack of health education, accessibility to specialists). Poor socioeconomic status and improper nutrition are contributing factors. Etiology Common in younger age group (school-going children). Both sexes, all ages affected. Inadequately treated/untreated AOM $\rightarrow$ tympanic membrane perforation $\rightarrow$ mucosal COM. Other causes: Traumatic perforation, grommet extrusion (perforation doesn't heal, permanent perforation). Permanent perforation: Outer epithelial layer and inner mucosal layer contact ("contact inhibition"). Infections (tonsils, adenoids, nasopharynx, nose, paranasal sinuses) $\rightarrow$ middle ear via ET $\rightarrow$ recurrent infection/discharge. Middle ear mucosa acts as shock organ for allergic reactions to ingested food/dust/hay $\rightarrow$ persistent otorrhea. Causative Organisms Most common: $P$. aeruginosa. Other: Proteus, $E$. coli, $S$. pneumoniae, $S$. aureus. Bacterial biofilms on middle ear mucosa play major role in chronic ear infections. Pearl Biofilms: Survival mechanism for bacteria. Organisms enveloped in extracellular polysaccharide matrix. Difficult for antibiotics to penetrate, cause antibiotic resistance. Clinical Features Symptoms Mucoid, non-foul-smelling, painless, non-blood-stained ear discharge. Discharge may be profuse, intermittent. Aggravates with upper respiratory infections, cold, water entry. Reduces with medication. Causes for intermittent/persistent discharge: Anteriorly: Sinonasal infection, nasopharyngeal infection (adenoids), upper respiratory allergy. Laterally (through perforation): Water entry, foreign body, cotton buds. Posteriorly: Mastoid reservoir of infection. Middle ear: Resistant organisms (rule out tuberculous otitis media). Bacterial biofilms may cause persistent discharge (resistance to antibiotics). Poor patient compliance. Systemic causes: Diabetes, immunocompromised states. Hearing loss: Usually conductive, mild to severe. Round window shielding effect: Patient hears better with discharge (maintains phase differential). Dry ear $\rightarrow$ sound strikes round and oval windows simultaneously, cancelling effect. Slowly progressive conductive hearing loss (tympanosclerosis or fibrosis involving ossicular chain). Mixed hearing loss (bacterial toxins, cytokines, ototoxic drugs absorbed into cochlea). Tinnitus (loss of ambient sound, bacterial toxins, ototoxic drugs affecting inner ear). Otalgia: Not common. Usually due to otitis externa secondary to discharge. Signs Perforation of tympanic membrane: Usually central. May be anterior, inferior, or posterior to malleus handle. Varying size. Middle ear mucosa may be pale pink/moist (inactive) or congested/edematous (active). Polyp may be seen. Otomysosis in external auditory canal (secondary to ear discharge or overuse of quinolone/steroid ear drops). Polyp: Pale, smooth, glistening mass of edematous mucosa protruding through perforation into external auditory canal. May be congested, covered in discharge with active infection. Ossicular chain: Usually intact/normal. In long-standing cases, erosion of ossicles (commonly long process of incus). Tympanosclerosis: White chalky deposits over tympanic membrane, ossicles, promontory, tendons, joints $\rightarrow$ conductive hearing loss. External auditory canal may be filled with discharge, dried discharge, otomycosis debris. Canal may be edematous (secondary otitis externa). Investigations Pure Tone Audiometry: Assesses degree/type of hearing loss. Documents hearing loss, compares postoperative to preoperative. If conductive hearing loss (air-bone gap) >40 dB, suspect ossicular chain involvement. Patch Test: Performed when air-bone gap >40 dB. Cigarette paper/filter paper covers perforation. Liquid paraffin on margins helps placement. PTA repeated. If hearing improves, ossicular chain is not involved. If worsening, ossicular discontinuity (tympanoplasty needed). If no change, test not done properly or ossicular fixity (tympanosclerosis/fibrosis). Culture and Sensitivity of Ear Discharge: Organisms usually $P$. aeruginosa, Proteus, $E$. coli, $S$. aureus, Bacteroides, anaerobic streptococci. Swab taken from middle ear after cleaning external auditory canal. X-Ray of the Mastoid: Prior to planned mastoid antrum opening or cortical mastoidectomy. Gives information on mastoid type, level of dural plate, sinus plate. Chronic middle ear disease often shows secondary sclerotic mastoid. High-Resolution CT Scan of the Temporal Bone: Used when mastoid reservoir of infection suspected. Rare complications of mucosal disease: Contrast-enhanced MRI for intracranial pathology. Diagnostic Nasal Endoscopy: If nasal/paranasal sinus disease symptoms, as a source of infection. Treatment Aim Eliminate infection. Recreate barrier between tympanic cavity and external auditory canal. Restore hearing. Medical Management Aural Toilet: Removal of discharge/debris from external auditory canal. Dry mopping (cotton on Jobson-Horne probe, suction clearance). Wet mopping (saline-soaked cotton) for dried discharge/ear drops. Topical Ear Drops: Used in actively discharging ear. Instilled 3-4 times/day for up to 2 weeks. High drug concentration, low MIC, helpful for resistant organisms. Combined with steroids (anti-inflammatory). Common drops: Quinolones (ciprofloxacin, ofloxacin) with dexamethasone. 1.5% acetic acid drops create acidic medium, eliminates $P$. aeruginosa. Instillation: Patient supine, affected ear upward. Instill drops, press tragus intermittently (tragal pumping). Stop if ear becomes dry. Note: May cause local allergy, skin maceration, fungus growth, resistance. Long-term quinolone/steroid drops $\rightarrow$ otomycosis. Avoid ototoxic drugs. Systemic Antibiotics: Used when topical drops fail or cannot reach infected areas (mastoid air cells). Started when infection source outside middle ear cleft (tonsillitis, adenoiditis, rhinosinusitis). Culture/sensitivity tests required. Precautions Avoid water entry into ear (cotton with Vaseline/sterile ear plugs), avoid swimming. Avoid forceful nose blowing (prevent infections from nasopharynx to middle ear). Discourage earbuds. Surgical Treatment Removal of Aural Polyps or Granulation Tissue: Removed before local medical therapy to allow topical antibiotics to reach middle ear. Removed carefully, not avulsed (may be attached to stapes, facial nerve, horizontal semicircular canal). Avulsion can result in giddiness, SNHL, facial nerve palsy, labyrinthitis. Cortical Mastoidectomy: When mastoid reservoir of infection is present. Some advocate for ETD (mastoid acts as buffer). Reconstructive Surgery: Various procedures to close tympanic membrane defect and improve hearing (myringoplasty, tympanoplasty). Myringoplasty: Surgical repair of tympanic membrane. Tympanoplasty: Surgical procedure to eradicate disease from middle ear and reconstruct hearing mechanism. Points to Ponder OME: Common in children, hearing loss due to fluid accumulation. Ear discharge: Common complaint, nature of discharge aids diagnosis. Mucoid/mucopurulent discharge in external auditory canal $\rightarrow$ tympanic membrane perforation (mucoid discharge from mucous glands/goblet cells). AOM: Common in infancy/early childhood due to ET anatomy (shorter, wider, more horizontal). COM: Mucosal or squamous. Both active/inactive. Old terminology: CSOM (TTD, AAD). TTD now mucosal, AAD now squamous. CSOM-TTD: Safe type, not usually associated with complications. CSOM-AAD: Dangerous type, can cause complications due to cholesteatoma. Cholesteatoma: Sac lined by squamous epithelium with central keratin mass. Bone-eroding properties, causes complications. Complications of CSOM: Intratemporal, extratemporal, intracranial. Chronic Otitis Media–Squamous Type or Chronic Suppurative Otitis Media-AAD Introduction Chronic inflammatory condition of middle ear cleft, usually involving posterosuperior part of mesotympanum, attic, antrum. Associated with entrapment of keratinizing squamous epithelium (cholesteatoma) in middle ear space, which can erode and destroy adjacent temporal bone tissues. Also known as: CSOM-AAD, Unsafe ear, Dangerous type of CSOM. Hallmark: Cholesteatoma or granulations. Higher risk of complications. Pearl Differential diagnosis of a blue drum: Hemotympanum, Glomus tympanicum, High jugular bulb with dehiscent floor of tympanic cavity, Cholesterol granuloma, Middle ear effusion. Complications of Otitis Media Occur when normal middle ear barriers are overcome, permitting infection spread to adjacent structures. Distinguished from sequelae (tympanosclerosis, atelectasis, adhesive otitis media, ossicular erosion, perforation, cholesteatoma formation, hearing loss) which are direct results of disease process, not acute emergencies. Complications can occur due to AOM or squamous COM (atticoantral type). Less common in mucosal COM. Factors favoring development: Bacteria with high virulence and antibiotic resistance. Patient factors: Age, immunosuppression, malnutrition, systemic diseases (tuberculosis, diabetes mellitus, malignancy). Inadequate treatment: Inadequate course/dose of antibiotics, wrong choice, lack of compliance. Poorly pneumatized mastoid. Pathophysiology and Routes of Spread Extension through bone (demineralized during acute infection, resorption by cholesteatoma/osteitis in chronic disease). Retrograde thrombophlebitis or periphlebitis of small veins through bone/dura to venous sinuses. Through normal anatomical pathways: Oval and round window to inner ear. Cochlear or vestibular aqueducts. Dehiscence of thin bony covering of jugular bulb. Dehiscence of tegmen tympani. Dehiscence of suture lines of temporal bone. Through nonanatomical defects (accidental/surgical trauma, neoplastic erosion). Through other surgical defects (vestibular opening from stapedectomy/lateral semicircular canal fenestration). Extension into brain tissue along periarteriolar spaces of Virchow-Robin. Squamous COM can cause complications due to bone-eroding properties of cholesteatoma. Table 8.3 Complications produced by squamous chronic otitis media Intratemporal Extratemporal Intracranial Acute coalescent mastoiditis Masked mastoiditis Acute petrositis Facial paralysis Labyrinthitis Postauricular abscess Bezold's abscess (sternomastoid) Zygomatic abscess Luc's abscess (meatal) Citelli's abscess (digastric) Parapharyngeal abscess Retropharyngeal abscess Meningitis Lateral sinus thrombophlebitis Extradural abscess Subdural abscess Brain abscess: temporal lobe/cerebellum Otitic hydrocephalus Intratemporal Complications Acute Mastoiditis Most suppurative middle ear infections have some mastoid air cell inflammation (proximity and mucosal continuity). Mastoiditis with osteitis: Infection spreads from mucosa to bony walls of mastoid air cell system. Breakdown of cells $\rightarrow$ acute coalescent mastoiditis (acute surgical mastoiditis). Predisposing Factors More common in children. Associated with reduced host resistance (malnutrition, immunosuppression, exanthematous fever, diabetes mellitus). Usually occurs in cellular mastoid. Causative Organisms $S$. pneumoniae, $\beta$-hemolytic streptococci, $H$. influenza. Occasionally gram-negative organisms (Pseudomonas, Proteus, $E$. coli). Pathogenesis Flowchart 8.2 depicts pathogenesis of acute mastoiditis. Clinical Features Classically occurs 2 weeks after otorrhea onset. Symptoms similar to AOM. Examination: Tympanic membrane perforation, conductive hearing loss. Constitutional symptoms: Fever, malaise, toxic look. Flowchart 8.2 Pathogenesis of acute mastoiditis Hyperaemia and edema of mucoperiosteal lining of mastoid air cells Obstruction/narrowing of aditus Thickened mucous membrane, impaired ciliary function and impaired drainage of middle ear through eustachian tube Venous stasis and local acidosis Dissolution of calcium from bony septae, increased osteoclastic activity in inflamed periosteum Hyperaemic decalcification Air cells coalesce into a larger cavity filled with purulent exudate and markedly thickened vascular mucoperiosteal granulations Table 8.4 Suggestive and definitive symptoms and signs (Acute Mastoiditis) Otorrhea persisting beyond 2 wk Presence of postauricular abscess Persistent or recurrent pain behind the ear Erythema and edema over the mastoid tip Mastoid tenderness and swelling over the mastoid region—ironed out mastoid Sagging of the posterosuperior meatal wall resulting from thickening of the periosteum of the bony external auditory meatus Investigations Complete blood count: Polymorphonuclear leukocytosis, raised ESR. Swab of discharge: For culture and sensitivity. Clean ear canal, swab from discharge through perforation. X-ray of mastoids (lateral oblique Schuller's view): Diffuse clouding of air cells (fluid replacement), destruction of bony septal walls. HRCT of temporal bone: Haziness of air cells, loss of bony trabeculae within mastoid process. Differential Diagnosis Postauricular suppurative lymphadenitis. Otitis externa: Furunculosis of external auditory canal involving posterior canal wall. Treatment High-dose intravenous antibiotics (culture/sensitivity report). Myringotomy to facilitate drainage of pus (if no perforation). Cortical mastoidectomy: To exenterate all accessible mastoid air cells if: Subperiosteal abscess. Sagging of posterosuperior meatal wall. Positive reservoir sign (persistent discharge after cleaning). No change/worsening after 48 hours of antibiotics. Mastoiditis with complications (facial nerve palsy, labyrinthitis, intracranial). Complications Subperiosteal abscess. Petrositis. Facial nerve paralysis. Labyrinthitis. Lateral sinus thrombophlebitis. Extradural abscess. Brain abscess. Otitic hydrocephalus. Subperiosteal Abscess Postauricular Abscess or Wilde's Abscess: Hematogenous spread of infection through minute vascular channels in suprameatal triangle. Abscess displaces pinna forward, outward, downward. Presents in subperiosteal plane, subcutaneous tissue, or open up with discharge from mastoid cutaneous fistula. Zygomatic Abscess: Infection in zygomatic air cells erodes through cortical bone at zygoma. Swelling above and in front of ear. Meatal or Luc's Abscess: Pus breaks through bony wall of antrum, external auditory meatus. Swelling visible in deep part of bony meatus. Citelli's Abscess: Pus travels along mastoid emissary vein or occipitotemporal suture $\rightarrow$ swelling posterior to mastoid. Pus can also track along posterior belly of digastric muscle from mastoid tip, anteriorly. Bezold's Abscess: Pus breaks through medial side of mastoid tip $\rightarrow$ tracks down beneath sheath of sternocleidomastoid muscle into neck. Treatment Intravenous antibiotics, followed by incision and drainage of abscess, and cortical mastoidectomy. Masked Mastoiditis Synonyms: Latent mastoiditis, subacute mastoiditis. Mastoiditis without draining ear or other usual signs/symptoms. Slow destruction of mastoid air cells without acute signs/symptoms. Often seen in acute mastoiditis modified by antibiotics. Clinical features: Mild pain over mastoid, persistent conductive hearing loss, thick tympanic membrane. Radiograph: Extensive decalcification and coalescence of mastoid air cells. Treatment: Cortical mastoidectomy. Antibiotics (culture/sensitivity). Granulation tissue, dark gelatinous material seen during mastoidectomy. Petrositis Infection spreads from middle ear and mastoid to petrous part of temporal bone (anterior/posterior petrous apex). Etiology Usually associated with acute coalescent mastoiditis, latent mastoiditis, cholesteatoma. Common causative organisms: Pneumococcus, $H$. influenza, $\beta$-hemolytic streptococci. Pathology Petrous apex related to abducens nerve and trigeminal ganglion. Pneumatized in 30% of individuals. Two groups of air cells to petrous apex: Posterosuperior tract: Starts in attic/antrum, runs around semicircular canals to petrous apex. Anteroinferior tract: Starts in hypotympanum, passes around ET/cochlea to petrous apex. Infection spreads along these tracts, can involve abducens nerve (Dorello's canal) and trigeminal ganglion (Meckel's cave). Clinical Features Gradenigo's Syndrome: Lateral rectus palsy (paralysis of sixth cranial nerve) $\rightarrow$ diplopia. Deep seated retro-orbital pain (trigeminal ganglion involvement). Persistent otorrhea. Other clinical features: Transient facial paresis, mild recurrent vertigo, low-grade intermittent fever, vomiting, headache. Investigations HRCT scan of temporal bone: Haziness in petrous apex cells. MRI: Better defines involvement of cells, abducens nerve, trigeminal ganglion. Better delineates spread to cavernous sinus. Swab for culture and sensitivity. Treatment High-dose antibiotics for 5-7 days, followed by complete mastoidectomy. If disease persists, petrous apex approached surgically to clear disease (transcochlear or translabyrinthine approach, affects hearing). Labyrinthitis Infection spreads to inner ear, causing labyrinthitis. In AOM, bacterial toxins enter inner ear through oval/round windows. Other predisposing factors: Mondini malformation, labyrinthine fistula (CT scan). Bone erosion (usually lateral semicircular canal) by cholesteatoma $\rightarrow$ labyrinthine fistula. Symptoms: Recurrent/transient vertigo, fluctuating SNHL. Nystagmus with positive fistula sign. HRCT temporal bone: Bony erosion of lateral semicircular canal. Infection spread from labyrinth to subarachnoid space via cochlear aqueduct $\rightarrow$ meningitis. Infection spread from meningitis into labyrinth. Treatment: Antibiotics, labyrinthine sedatives. Steroids. Canal wall down mastoidectomy for disease clearance in cholesteatoma. After complete cholesteatoma removal, fistula covered by graft (if not, sac everted to epithelialize). Facial Nerve Paralysis Can occur in AOM or with cholesteatoma. AOM: Occurs within 2 weeks of onset. Due to inflammatory edema (compression in fallopian canal) or irritation of nerve (osteitis). Exposure of dehiscent facial nerve segment (tympanic) to active infection $\rightarrow$ direct irritation. Cholesteatoma: Erosion of bony fallopian canal $\rightarrow$ nerve exposure to active infection, compression, invasion. Management Facial palsy following AOM: Myringotomy to release pus, antibiotics. Mastoidectomy indicated if: Paralysis 2 weeks after AOM onset. In patients with COM. Paralysis fails to resolve after adequate management of otitis media. ENoG indicates >90% motor nerve fiber degeneration within 6 days of onset. Exploration of facial canal, removal of granulations. Cholesteatoma: Modified radical mastoidectomy with complete cholesteatoma removal, with/without facial nerve decompression (depending on MRI/intraoperative findings). Intracranial Complications Extradural Abscess Synonym: Epidural abscess. Collection of pus between bone and dura. Can occur due to AOM or cholesteatoma. May precede brain abscess, coexist with sinus thrombophlebitis. Pathology Overlying dural bone destroyed by hyperemic decalcification (AOM) and enzymatic activity (cholesteatoma) $\rightarrow$ pus collection in epidural space. Affected dura covered with granulation, appears unhealthy/discolored. May lie in middle cranial fossa, posterior cranial fossa, or as perisinus abscess (outside dura of lateral venous sinus). Clinical Features Some cases asymptomatic, discovered accidentally during mastoidectomy. Persistent headache (disappears with free flow of pus from ear). Differential Diagnosis Postauricular suppurative lymphadenitis. Otitis externa: Furunculosis of external auditory canal involving posterior canal wall. Diagnosis Contrast-enhanced CT or MRI shows dural elevation. Treatment Antibiotic therapy (before and after surgery). Mastoidectomy: Overlying bone removed until healthy dura. If strong suspicion, remove overlying intact tegmen tympani bone to check/evacuate pus. Observe closely for other intracranial complications. Treat primary disease. Subdural Abscess Collection of pus in subdural space (between dura and arachnoid mater). Rare, fatal in pre-antibiotic era. Pathology Infection spreads by bone/dura erosion or thrombophlebitic process. Pus in subdural space against cerebral hemisphere $\rightarrow$ pressure symptoms. Later, loculated in subdural space, may rupture. Clinical Features Sudden, severe, progressive. Severe, throbbing headache with fever, vomiting, rapid deterioration $\rightarrow$ subdural abscess. Clinical features due to: Meningeal irritation, cortical vein thrombophlebitis, raised CSF pressure. Meningeal irritation: Headache, high-grade fever, malaise, progressive drowsiness, neck rigidity, Kernig's sign. (May be masked by prior antibiotics). Cortical vein thrombophlebitis/cerebrum: Aphasia, contralateral hemiplegia/hemianopia, seizures. Raised CSF pressure: Papilledema, ptosis, dilated pupils (third cranial nerve involvement). Other cranial nerves may be involved. Diagnosis MRI superior to CT scan. Distinguishes epidural/subdural abscess. CT scan shows a loculated subdural abscess. Lumbar puncture contraindicated (cerebellar tonsil herniation risk). Treatment Surgical emergency. Burr holes to drain abscess. High-dose broad-spectrum intravenous antibiotics. Mastoidectomy after abscess resolves and patient improves. Otogenic Brain Abscess Focal suppurative infection of brain parenchyma. ~50% of brain abscesses in adults, 25% in children are otogenic. Adults: Usually follows CSOM with cholesteatoma. Children: Usually result of AOM. Cerebral abscesses (temporal lobe) more frequent than cerebellar. Bimodal age distribution (pediatric, fourth decade). Route of Infection Direct extension of middle ear infection or retrograde thrombophlebitis of dural vessels. Often associated with extradural abscess. Cerebellar abscess from direct extension through retrograde thrombophlebitis from sigmoid sinus (related to posterior mastoid wall). Bacteriology Both aerobic and anaerobic organisms. Polymicrobial cultures influenced by host immune status. Aerobic: Pyogenic staphylococci, $S$. pneumoniae, $S$. haemolyticus, gram-negative bacteria ($P$. mirabilis, $E$. coli, $P$. aeruginosa). Anaerobic: Peptostreptococcus, $B$. fragilis. $H$. influenza found rarely. Pathogenesis Develops through four stages. Invasion (initial encephalitis): Mild symptoms (headache, low-grade fever, malaise, drowsiness). May go unnoticed. Lasts 1-3 days. Localization (latent abscess): Pus localizes with capsule formation. Patients asymptomatic for days/weeks. Lasts 4-10 days. Enlargement (manifest abscess): Abscess enlarges. Edema zone around abscess $\rightarrow$ symptom aggravation. Clinical features due to raised intracranial tension, cerebral/cerebellar dysfunction. Lasts 10-13 days. Termination (rupture of abscess): Expanding abscess in white matter ruptures into ventricle/subarachnoid space $\rightarrow$ fatal meningitis. Clinical Features Often associated with other complications (extradural abscess, perisinus abscess, meningitis, sigmoid sinus thrombosis, labyrinthitis). Clinical picture can overlap. Patient appears toxic, drowsy. Dizziness, nystagmus, vomiting, ataxia (cerebellar abscess). Temporal abscess may cause seizures. Clinical features due to raised intracranial tension or affected brain area (localizing features). Symptoms and Signs of Raised Intracranial Tension Headache: Severe, generalized, worse in morning. Nausea and projectile vomiting (more often cerebellar). Consciousness alters: Lethargy $\rightarrow$ drowsiness, confusion, stupor, coma. Papilledema: Absent early. Appears late if intracranial tension persists >2-3 weeks. Appears early in cerebellar abscess. Slow pulse, subnormal temperature. Localizing Features of a Temporal Lobe Abscess Nominal aphasia: Lesion in dominant cerebral hemisphere (left in right-handed). Cannot name objects, but explains use. Contralateral homonymous hemianopia: Pressure on optic radiations. Visual field defect usually upper quadrant, recorded by perimetry. Confrontation test (patient's visual field vs. examiner's). Contralateral motor paralysis: Upward spread causes facial palsy, then arm/leg paralysis. Inward spread to internal capsule leads to leg, then arm/face paralysis. Epileptic fits: Small involuntary smacking lip/tongue movements. Generalized fits may occur. Localizing Features of a Cerebellar Abscess Suboccipital headache with neck rigidity. Spontaneous nystagmus. Ipsilateral ataxia: Staggering to side of lesion. Finger-nose test: Past pointing, intention tremor. Dysdiadochokinesia: Rapid pronation/supination movements become slower/irregular on affected side. Investigation Contrast-enhanced CT scan: Confirms site/size of abscess. Detects associated complications (extradural abscess, sigmoid sinus thrombosis). Ring sign: Brain abscess appears as hypodense area surrounded by edema. Temporal bone better visualized on CT. MRI: Detects subtle changes in brain parenchyma, spread of abscess. Lumbar puncture: Rise in pressure, increased protein, normal sugar, raised WBCs (polymorphs or lymphocytes). (Depends on infection severity). Medical Treatment Intravenous antibiotics: Chloramphenicol, penicillin, derivatives. Metronidazole for anaerobes. Aminoglycosides (gentamicin) for pseudomonas/proteus. Antibiotics changed per culture/sensitivity. Dexamethasone: 4 mg IV q6h. Mannitol: 20% at 0.5 g/kg body weight. Both reduce edema and intracranial tension. Surgical Treatment Life-saving neurosurgical intervention is more important than otological management. Aspiration of pus for culture/sensitivity. Repeat CT/MRI for resolution. Repeated aspirations may be done. If not decreasing/rapidly enlarging, excision needed. After aspiration, penicillin instilled into abscess. Otological Intervention Once neurologically stable, tympanomastoid surgery. Cholesteatoma requires modified radical mastoidectomy. Meningitis Inflammation of leptomeninges (pia and arachnoid) and CSF of subarachnoid space. Most common intracranial complication. Can occur in children and adults. Causes After AOM episode in children. Squamous COM disease. Temporal bone fracture causing CSF leak. Following middle ear or mastoid surgeries (rare). Route of Spread Infection from middle ear/mastoid can reach meninges via: Preformed pathways via patent petrosquamous suture. Retrograde venous thrombophlebitis. Direct erosion of bone and dura. From labyrinthitis via cochlear aqueduct. Commonest organisms: $H$. influenzae, $S$. pneumoniae. Clinical Features Severity varies with infection extent. Earliest symptoms: High-grade fever with chills/rigors. Throbbing headache, photophobia. Nausea, sometimes projectile vomiting. Irritability, restlessness. Infants may develop seizures. Signs (may be masked by antibiotics): Neck rigidity (earliest). Kernig's sign: Leg extension with thigh flexion on abdomen is painful. Brudzinski's sign: Neck flexion results in hip/knee flexion. Cranial nerve palsies, hemiplegia. Exaggerated deep tendon reflexes initially, then sluggish/absent. Investigations HRCT temporal bone: Imaging modality of choice. Shows bony erosion, congenital malformations, fistulas. MRI: Rules out inflammatory changes in brain. Lumbar puncture/CSF analysis: Establishes diagnosis. Cloudy/yellow (xanthochromic). Raised cell count (polymorphs predominance). Raised protein level. Low sugar, chlorides. Gram staining/culture: CSF sensitivity to identify organism, antibiotic sensitivity. Fundoscopy: Indistinct disc margins, choking of vessels. Ear swab for culture/sensitivity. Treatment Medical treatment takes precedence. Surgery for failed medical therapy. Antibiotics: Crystalline penicillin, ampicillin, chloramphenicol, third-generation cephalosporins (IV for 7-10 days). Surgery when patient condition improves. AOM: Myringotomy with/without cortical mastoidectomy. Cholesteatoma: Modified radical mastoidectomy. Lateral Sinus Thrombophlebitis Also known as: Sigmoid sinus thrombosis. Inflammation of inner wall of lateral sinus with thrombus formation, later infected. Incidence decreased due to newer antibiotics; mortality remains high. Etiology Acute coalescent mastoiditis. Masked mastoiditis. Cholesteatoma. Common bacteriology: $\beta$-hemolytic Streptococcus, Pneumococcus, Bacillus, Proteus, Pseudomonas. Clinical Features Fever: Hectic picket fence type, chills, rigors. One/more peaks/day, doesn't touch baseline (septic emboli release). Later, temperature fall with profuse sweating, well-being sense. Headache: Mild (perisinus abscess). May get severe with intracranial pressure increase. Deep-seated ear pain, ear discharge. Griesinger's sign: Thrombosis of mastoid emissary vein $\rightarrow$ tenderness/edema over posterior mastoid. Pathognomonic for sigmoid sinus thrombosis. Tenderness along internal jugular vein (neck) due to thrombosis. Enlarged/tender jugular lymph nodes. Anemia. Papilledema: Fundus shows blurring of disc margins, retinal hemorrhages, dilated veins. Occurs when clots extend to superior sagittal sinus. Crowe-Beck test (Lily-Crowe sign): Pressure on opposite internal jugular vein $\rightarrow$ retinal/supraorbital vein engorgement, subsides on pressure release. Cavernous sinus thrombosis: Proptosis, ptosis, chemosis, ophthalmoplegia. Investigations Blood culture: Antibiotic changed per sensitivity. Peripheral smear: Rules out malarial parasites. Culture/sensitivity of ear discharge (if present). Lumbar puncture: Normal CSF findings with pressure rise. Rules out meningitis. Tobey-Ayer test: Records CSF pressure while compressing one/both jugular veins. Compression of affected side $\rightarrow$ no effect. Compression of opposite side $\rightarrow$ rapid CSF pressure rise. Contrast-enhanced CT scan: Typical feature of sinus thrombosis is "delta sign" (empty triangular area with rim enhancement, central low density in sigmoid sinus). MRI (Gadolinium-enhanced): Thrombus appears as soft-tissue signal with vascular/bright dural walls. More sensitive than CT. MR angiography/venography: Demonstrates thrombus by radiology. Complications If untreated: Septicemia, meningitis, brain abscess. Septic thrombi $\rightarrow$ pyogenic abscess in lungs, bones, joints, subcutaneous tissues. Thrombosis of jugular bulb/vein $\rightarrow$ cranial nerves IX-XI involvement. Cavernous sinus thrombosis, otitic hydrocephalus. Treatment Antibiotics (1 million units IM crystalline penicillin q6h) for pyogenic organisms. For 10-14 days per culture/sensitivity. Mastoidectomy: Cortical or modified radical mastoidectomy in AOM/cholesteatoma. Bony sinus plate removed to expose dura, drain perisinus abscess. Ligation of internal jugular vein: If medical/surgical options fail (restricts thromboemboli spread). Blood transfusion for anemia. Improve general well-being (supportive/nutritional therapy). Anticoagulants: May help reduce clot propagation, promote sinus recanalization, reduce neurological deficits. Otitic Hydrocephalus Also known as: Benign raised intracranial hypertension. No associated ventricular dilation. Rare complication. Characterized by raised intracranial pressure, normal CSF. Seen in children/adolescents. Mechanism Causes of obstruction to venous return. Reduced CSF absorption. Clinical Features Severe headache (usual presenting complaint), associated with nausea, vomiting. Traction on sixth cranial nerve $\rightarrow$ diplopia. Increased intracranial pressure $\rightarrow$ papilledema, optic atrophy $\rightarrow$ blurring of vision. Papilledema may be accompanied by exudates/hemorrhages. Nystagmus. Diagnosis MRI to evaluate venous sinuses. Lumbar puncture: CSF sterile, normal cell count/sugar/protein. Pressure raised to ~300 mm water (normal 70-120 mm). Treatment Medical: Reduce CSF pressure (corticosteroids, mannitol, acetazolamide). Surgical: Reduce CSF pressure, prevent optic atrophy/blindness (lumbar drain, repeated lumbar puncture, lumboperitoneal shunt). Mastoidectomy, decompression of sigmoid sinus. Optic sheath decompression may prevent optic atrophy.