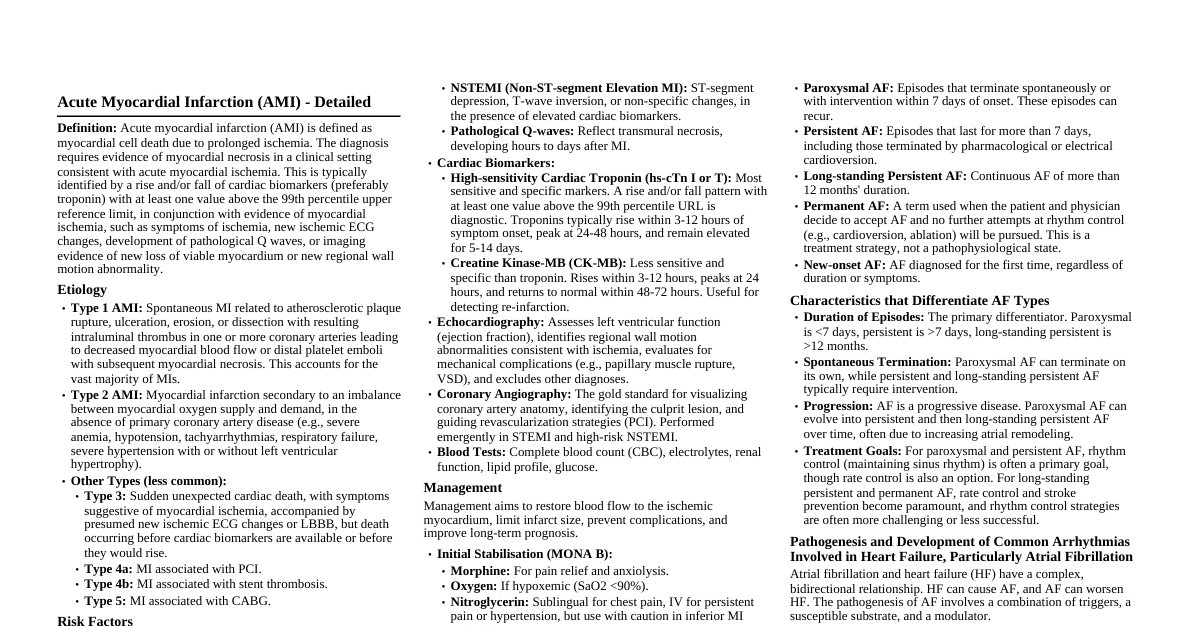
Acute Myocardial Infarction (AMI) Definition: Myocardial cell death due to prolonged ischemia. Diagnosed by rise/fall of cardiac biomarkers (troponin) with evidence of myocardial ischemia. Etiology: Atherosclerosis (most common), coronary artery spasm, coronary embolism, vasculitis, cocaine use. Risk Factors: Hypertension, hyperlipidemia, diabetes mellitus, smoking, obesity, family history, age, male sex. Mechanism: Usually rupture of an atherosclerotic plaque leading to thrombus formation, occluding a coronary artery. Clinical Features: Chest pain (crushing, substernal, radiating to arm/jaw, >20 min), dyspnea, diaphoresis, nausea, vomiting, syncope. Investigations: ECG: ST-elevation (STEMI), T-wave inversion, Q-waves, ST-depression (NSTEMI). Cardiac Biomarkers: Troponin I/T (rise and fall, peak 12-24h). Echocardiography: Wall motion abnormalities, EF. Coronary Angiography: Gold standard for identifying culprit lesion. Management: Acute (MONA BASH): Morphine, Oxygen, Nitrates, Aspirin, Beta-blockers, ACE inhibitors, Statins, Heparin. Reperfusion: Percutaneous Coronary Intervention (PCI) within 90-120 min or Fibrinolysis within 30 min (if PCI unavailable). Secondary Prevention: Antiplatelets (DAPT), statins, ACEI/ARB, beta-blockers, lifestyle modification. Complications: Arrhythmias, heart failure, cardiogenic shock, mechanical complications (VSD, papillary muscle rupture), pericarditis (Dressler's syndrome), ventricular aneurysm. Atrial Fibrillation (AF) Definition: Supraventricular tachyarrhythmia characterized by uncoordinated atrial activation and consequently ineffective atrial contraction. Types: Paroxysmal: Terminates spontaneously within 7 days. Persistent: Lasts >7 days, requires intervention to terminate. Long-standing Persistent: Lasts >12 months. Permanent: Accepted by patient/physician, no further attempts to restore sinus rhythm. Pathogenesis: Multiple re-entrant wavelets in the atria, often triggered by ectopic beats from pulmonary veins. Electrical and structural remodeling perpetuates AF. Management: Rate Control: Beta-blockers, calcium channel blockers (diltiazem, verapamil), digoxin. Goal: HR Rhythm Control: Cardioversion (electrical or pharmacological), antiarrhythmic drugs (amiodarone, flecainide), catheter ablation. Anticoagulation (Stroke Prevention): CHA$_2$DS$_2$-VASc score guided (NOACs preferred over warfarin). Difference between Atrial Flutter and AF: Feature Atrial Fibrillation Atrial Flutter Atrial Activity (ECG) Irregularly irregular, chaotic fibrillatory waves (f-waves) Sawtooth pattern (F-waves), regular atrial rate (250-350 bpm) Ventricular Response Irregularly irregular Usually regular (e.g., 2:1, 3:1 block), can be variable Mechanism Multiple re-entrant wavelets Single re-entrant circuit (usually cavotricuspid isthmus) Infective Endocarditis (IE) Etiology: Bacterial (most common: Staph. aureus, Strep. viridans, Enterococci), fungal. Risk Factors: Prosthetic heart valves, congenital heart disease, IV drug use, previous IE, poor dental hygiene, indwelling catheters. Pathogenesis: Endothelial damage $\rightarrow$ sterile thrombus formation $\rightarrow$ bacteremia $\rightarrow$ bacterial adherence $\rightarrow$ vegetation formation. Clinical Features: Fever (most common): >90% of cases. Heart Murmur: New or worsening. Systemic Emboli: Stroke, splenic infarct, Janeway lesions (painless, palms/soles), Osler's nodes (painful, fingers/toes). Immunological Phenomena: Glomerulonephritis, Roth spots (retinal hemorrhages). Splenomegaly, clubbing. Diagnosis: Modified Duke Criteria (blood cultures, echocardiography). Management: Antibiotics: Prolonged IV antibiotics (4-6 weeks), guided by blood cultures/sensitivity. Empiric therapy if cultures pending. Surgery: For heart failure, uncontrolled infection, large vegetations, recurrent emboli, abscess formation. Prevention/Prophylaxis: Dental procedures: For high-risk patients (prosthetic valves, previous IE, certain congenital heart diseases) with specific procedures. Maintain good oral hygiene. Acute Rheumatic Fever (ARF) Etiology: Autoimmune inflammatory reaction to Group A Streptococcus (GAS) pharyngitis. Pathogenesis: Molecular mimicry; antibodies against GAS antigens cross-react with host tissues (heart, joints, brain, skin). Clinical Features: (Modified Jones Criteria) Major Criteria: Carditis: Pericarditis, myocarditis, endocarditis (new murmur, cardiomegaly, CHF). Polyarthritis: Migratory, large joints. Chorea (Sydenham's): Involuntary, purposeless movements. Erythema Marginatum: Non-itchy, pink rings with clear centers. Subcutaneous Nodules: Painless, over bony prominences. Minor Criteria: Arthralgia, fever, elevated ESR/CRP, prolonged PR interval on ECG. Diagnostic Criteria: Evidence of preceding GAS infection (ASO titer, throat culture) PLUS 2 major OR 1 major and 2 minor criteria. Management: Antibiotics: Penicillin to eradicate GAS (e.g., Benzathine Penicillin G). Anti-inflammatory: Aspirin for arthritis, corticosteroids for severe carditis. Supportive: Bed rest. Prophylaxis: Long-term penicillin (monthly IM Benzathine Penicillin G) to prevent recurrent ARF and progression to Rheumatic Heart Disease. Duration depends on carditis presence. Congestive Cardiac Failure (CCF) / Heart Failure (HF) Definition: Inability of the heart to pump sufficient blood to meet metabolic demands, or to do so only at elevated filling pressures. Etiology: Coronary artery disease (most common), hypertension, valvular heart disease, cardiomyopathy, arrhythmias, diabetes, obesity. Clinical Features: Left-sided HF: Dyspnea (exertional, orthopnea, PND), cough, crackles, S3 gallop, pulmonary edema. Right-sided HF: Peripheral edema, JVD, hepatomegaly, ascites, nausea, anorexia. General: Fatigue, weakness, reduced exercise tolerance. Investigations: ECG: Underlying ischemia, hypertrophy, arrhythmias. Chest X-ray: Cardiomegaly, pulmonary congestion (Kerley B lines, pleural effusion). Echocardiography: Ejection Fraction (EF), chamber sizes, wall motion, valvular function. BNP/NT-proBNP: Elevated in HF, correlates with severity. Blood tests: Renal function, electrolytes, thyroid. Management: Lifestyle: Sodium restriction, fluid restriction, exercise. Pharmacological (HFrEF - reduced EF): ACE Inhibitors/ARBs: Reduce afterload, prevent remodeling. Beta-blockers: Reduce HR, improve contractility, anti-remodeling. MRAs (Spironolactone, Eplerenone): Diuresis, anti-fibrotic. SGLT2 inhibitors (Dapagliflozin, Empagliflozin): Recent evidence, mortality benefit. Diuretics (Loop): Symptomatic relief of congestion. ARNI (Sacubitril/Valsartan): For appropriate HFrEF patients, superior to ACEI. Devices: ICD (for sudden cardiac death prevention), CRT (for dyssynchrony). Heart Failure with Preserved Ejection Fraction (HFpEF): EF $\ge 50\%$. Heart is stiff, impaired relaxation (diastolic dysfunction). Often associated with hypertension, diabetes, obesity, older age. Treatment focuses on managing comorbidities and symptom relief (diuretics). SGLT2 inhibitors also show benefit. Hypertension Causes: Primary (Essential) Hypertension (90-95%): Idiopathic, multifactorial (genetics, lifestyle). Secondary Hypertension (5-10%): Identifiable cause. Renal: Renal artery stenosis, CKD, polycystic kidney disease. Endocrine: Primary aldosteronism, Cushing's syndrome, pheochromocytoma, thyroid disease. Vascular: Aortic coarctation. Drugs: OCPs, NSAIDs, decongestants, steroids. Clinical Signs & Symptoms: Often asymptomatic ("silent killer"). Symptoms usually appear with complications: headache (severe), dizziness, blurred vision, epistaxis, chest pain, dyspnea. Organ Manifestations (Target Organ Damage): Heart: LV hypertrophy, CAD, HF, arrhythmias. Brain: Stroke (ischemic/hemorrhagic), TIA, hypertensive encephalopathy, dementia. Kidneys: Nephrosclerosis, CKD. Eyes: Hypertensive retinopathy (arteriolar narrowing, hemorrhages, exudates, papilledema). Blood Vessels: Aneurysms, peripheral artery disease. Management: Lifestyle Modifications: Diet (DASH), exercise, weight loss, smoking cessation, reduced alcohol/sodium intake. Pharmacological: First-line: Thiazide diuretics, ACE inhibitors/ARBs, Calcium Channel Blockers. Second-line: Beta-blockers, alpha-blockers. Individualized based on comorbidities. Hypertensive Emergency: Severe hypertension (SBP >180 and/or DBP >120 mmHg) with acute target organ damage. Requires immediate IV antihypertensives (e.g., labetalol, nicardipine, nitroprusside) for gradual BP reduction. Hypertensive Urgency: Severe hypertension without acute target organ damage. Oral medications, gradual BP reduction over 24-48 hours. Mitral Regurgitation (MR) Aetiology: Primary (Organic): Valvular leaflet/chordal abnormality (e.g., myxomatous degeneration, IE, rheumatic heart disease, papillary muscle rupture). Secondary (Functional): Normal valve leaflets, but annular dilatation or ventricular remodeling prevents leaflet coaptation (e.g., ischemic cardiomyopathy, dilated cardiomyopathy). Clinical Features: Often asymptomatic for years. Dyspnea, fatigue, orthopnea, PND (due to left heart failure). Palpitations (due to AF). Murmur: Holosystolic, high-pitched, blowing, best heard at apex, radiating to axilla. S3 gallop. Management: Medical: Vasodilators (ACEI/ARBs), diuretics for symptom control. Rate control for AF. Surgical: Mitral valve repair (preferred) or replacement for severe symptomatic MR, or asymptomatic severe MR with LV dysfunction or new-onset AF. Complications: Left ventricular dysfunction, atrial fibrillation, pulmonary hypertension, heart failure. Angina Pectoris Definition: Chest pain or discomfort due to myocardial ischemia, usually provoked by exertion and relieved by rest or nitroglycerin. Risk Factors: Same as CAD (hypertension, hyperlipidemia, diabetes, smoking, obesity, family history, age). Clinical Features: Location: Substernal, retrosternal. Character: Pressure, tightness, squeezing, heaviness, burning. Radiation: Left arm, jaw, neck, back, epigastrium. Duration: 2-10 minutes. Precipitating factors: Exertion, cold weather, emotional stress, heavy meals. Relieving factors: Rest, sublingual nitroglycerin. Types: Stable Angina: Predictable, reproducible, relieved by rest/NTG. Unstable Angina: New onset, increasing in frequency/severity, occurs at rest, not relieved by NTG. Considered Acute Coronary Syndrome (ACS). Prinzmetal's (Variant) Angina: Caused by coronary artery spasm, often occurs at rest, usually without significant CAD. Management: Lifestyle: Risk factor modification (smoking cessation, diet, exercise). Pharmacological: Nitrates: Symptomatic relief (sublingual NTG) and prevention. Beta-blockers: Reduce HR and contractility, decrease myocardial oxygen demand. First-line for chronic stable angina. Calcium Channel Blockers: For patients intolerant to beta-blockers or with vasospastic angina. Antiplatelets (Aspirin): Reduce thrombotic events. Statins: Lipid lowering, plaque stabilization. ACE inhibitors: For patients with CAD and comorbidities. Revascularization: PCI or CABG for severe symptoms despite medical therapy, or high-risk anatomy. Mitral Stenosis (MS) Etiology: Almost always rheumatic heart disease. Less common: congenital, calcification. Symptoms: Dyspnea (exertional, orthopnea, PND) due to pulmonary congestion. Hemoptysis. Fatigue, reduced exercise tolerance. Palpitations (due to AF). Hoarseness (Ortner's syndrome - compression of recurrent laryngeal nerve). Signs: Murmur: Loud S1, opening snap, mid-diastolic rumble, best heard at apex in left lateral position. Malar flush (plethora). AF, signs of right heart failure (JVD, hepatomegaly, edema) in advanced cases. Management: Medical: Diuretics for pulmonary congestion, beta-blockers/calcium channel blockers for rate control in AF, anticoagulation for AF. Interventional: Percutaneous mitral balloon commissurotomy (PMBC) for suitable anatomy. Surgical: Mitral valve replacement or open commissurotomy for severe symptomatic MS not suitable for PMBC. Complications: Atrial fibrillation, pulmonary hypertension, right heart failure, systemic embolization (stroke). Cardiac Conduction System & AV Blocks Conducting System Diagram SA Node AV Node Bundle of His LBB RBB Purkinje Fibers Atrioventricular (AV) Blocks First-Degree AV Block: ECG: PR interval >0.20 seconds, constant. All P waves followed by QRS complex. Clinical: Asymptomatic, no treatment needed. Second-Degree AV Block: Mobitz Type I (Wenckebach): ECG: Progressive lengthening of PR interval until a P wave is blocked (no QRS). Cycle repeats. Clinical: Often asymptomatic, usually benign, may require pacemaker if symptomatic. Mobitz Type II: ECG: Constant PR interval for conducted beats. Intermittent P waves are blocked (no QRS). Clinical: More serious, higher risk of progression to Complete Heart Block. Often requires pacemaker. Third-Degree (Complete) AV Block: ECG: No association between P waves and QRS complexes (AV dissociation). Atrial rate > ventricular rate. Ventricular escape rhythm (slow, wide QRS if junctional/ventricular origin). Clinical: Syncope, dizziness, fatigue, heart failure. Requires permanent pacemaker. Cardiomyopathy Classification Dilated Cardiomyopathy (DCM): Clinical Features: Enlarged ventricles, impaired systolic function (reduced EF). Symptoms of heart failure (dyspnea, fatigue), arrhythmias. Etiology: Idiopathic, ischemic, viral, alcohol, genetic, peripartum. Treatment: HF management (ACEI, beta-blockers, diuretics), ICD for high-risk arrhythmias, heart transplant. Hypertrophic Cardiomyopathy (HCM): Clinical Features: LV hypertrophy (often asymmetrical), diastolic dysfunction, outflow tract obstruction (HOCM). Dyspnea, chest pain, syncope, sudden cardiac death (SCD). Etiology: Genetic (sarcomeric protein mutations). Treatment: Beta-blockers/CCBs (verapamil) to improve diastolic filling/reduce obstruction, ICD for SCD prevention, septal myectomy/alcohol ablation for severe obstruction. Restrictive Cardiomyopathy (RCM): Clinical Features: Rigid ventricular walls, impaired diastolic filling, normal systolic function. Symptoms of right heart failure (edema, JVD), dyspnea. Etiology: Infiltrative diseases (amyloidosis, sarcoidosis, hemochromatosis), fibrosis. Treatment: Treat underlying cause, diuretics for symptom relief. Prognosis often poor. Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC): Clinical Features: Fibrofatty replacement of RV myocardium, leading to RV dilatation and dysfunction. Ventricular arrhythmias, SCD, right heart failure. Etiology: Genetic (desmosomal protein mutations). Treatment: Antiarrhythmic drugs, ICD for SCD prevention, HF management. Hypertensive Left Ventricular Failure Clinical Features: Acute onset dyspnea, orthopnea, PND, cough (frothy sputum), chest pain, signs of pulmonary edema (rales, S3, elevated JVP), severe hypertension. Investigations: ECG: LV hypertrophy, ischemia. Chest X-ray: Cardiomegaly, pulmonary vascular congestion, alveolar edema, pleural effusions. Echocardiography: LV hypertrophy, impaired diastolic/systolic function, elevated filling pressures. BNP: Elevated. Treatment: Immediate: Oxygen, nitrates (IV), diuretics (IV furosemide), ACE inhibitors (IV enalaprilat) or other vasodilators (sodium nitroprusside) to reduce preload and afterload. Blood Pressure Control: Careful titration of antihypertensives to gradually reduce BP without causing hypoperfusion. Long-term: Management of underlying hypertension and chronic heart failure. Sick Sinus Syndrome (SSS) Definition: A group of arrhythmias caused by sinus node dysfunction, leading to inappropriate heart rates. Clinical Features: Syncope, presyncope, dizziness, fatigue, palpitations, dyspnea. Often asymptomatic. ECG Manifestations: Sinus bradycardia, sinus pauses/arrest, sinoatrial exit block, bradycardia-tachycardia syndrome (alternating bradycardia and supraventricular tachycardias like AF). Management: Asymptomatic: No treatment. Symptomatic: Permanent pacemaker (dual-chamber usually preferred). Treat any contributing medications (e.g., beta-blockers) if possible. Pericardial Effusion & Management Definition: Accumulation of fluid in the pericardial sac. Etiology: Pericarditis (viral, bacterial, autoimmune), malignancy, uremia, hypothyroidism, trauma, post-MI. Clinical Features: Can be asymptomatic. Large/rapid effusions can cause dyspnea, chest pain, distant heart sounds. In severe cases, cardiac tamponade. Diagnosis: Echocardiography (confirmatory). Chest X-ray (water bottle heart). Management: Small, asymptomatic: Observe, treat underlying cause. Moderate-Large, symptomatic: Pericardiocentesis (fluid drainage) or surgical pericardial window. Cardiac Tamponade: Medical emergency, requires urgent pericardiocentesis. Cardiopulmonary Resuscitation (CPR) Definition: Emergency procedure for cardiac arrest to maintain brain function until further measures are taken. Components (Adult BLS): Check for responsiveness & breathing. Call for help/AED. Chest Compressions: Hard and fast (100-120 bpm). Depth 2-2.4 inches (5-6 cm). Allow full chest recoil. Minimize interruptions. Airway: Head tilt-chin lift. Breathing: 2 rescue breaths after 30 compressions (30:2 ratio). Each breath 1 second, visible chest rise. Defibrillation: Use AED as soon as available. Follow prompts. Advanced Cardiac Life Support (ACLS): Includes advanced airway, IV access, medications (epinephrine, amiodarone), identification and treatment of reversible causes (H's and T's). Secondary Hypertension Causes: Renal: Renal artery stenosis, chronic kidney disease, polycystic kidney disease, glomerulonephritis. Endocrine: Primary aldosteronism (Conn's syndrome), Cushing's syndrome, pheochromocytoma, hyperthyroidism, hypothyroidism. Vascular: Coarctation of the aorta. Sleep Apnea. Drugs/Substances: Oral contraceptives, NSAIDs, corticosteroids, decongestants, cocaine, amphetamines, excessive alcohol. Clues for Secondary HTN: Early onset ( Ischemic Cardiomyopathy Definition: Dilated cardiomyopathy caused by extensive coronary artery disease, leading to chronic myocardial ischemia and/or multiple myocardial infarctions, resulting in LV dysfunction and dilation. Clinical Features: Symptoms of heart failure (dyspnea, fatigue), angina, arrhythmias. Diagnosis: Echocardiography (dilated LV, reduced EF, wall motion abnormalities), coronary angiography (severe CAD). Management: Similar to HFrEF (ACEI, beta-blockers, MRAs, SGLT2i), revascularization (PCI/CABG) if viable myocardium is present, ICD for SCD prevention. P-R Interval Definition: Interval on an ECG from the beginning of the P wave to the beginning of the QRS complex. Represents: Time taken for atrial depolarization and conduction through the AV node, Bundle of His, and Purkinje fibers. Normal Duration: $0.12 - 0.20$ seconds ($3-5$ small squares). Significance: Prolonged (>0.20s): First-degree AV block. Short ( Pre-excitation syndromes (e.g., Wolff-Parkinson-White syndrome). Variable: Second-degree Mobitz Type I AV block (Wenckebach). Treatment of Digitalis Toxicity Mechanism: Digoxin inhibits Na$^+$/K$^+$-ATPase, increasing intracellular Na$^+$ and subsequently intracellular Ca$^{2+}$, leading to increased contractility. Toxicity Symptoms: Cardiac: Arrhythmias (bradycardia, AV block, ventricular arrhythmias like VT/VF, bidirectional VT, atrial tachycardia with block), ectopic beats. Non-cardiac: Nausea, vomiting, anorexia, abdominal pain, visual disturbances (yellow-green halos), confusion. Management: Stop Digoxin. Correct Electrolytes: Hypokalemia exacerbates toxicity. Bradycardia/AV Block: Atropine, temporary pacing. Ventricular Arrhythmias: Lidocaine, phenytoin. Specific Antidote: Digoxin immune Fab (Digibind) for severe, life-threatening toxicity. Fallot's Tetralogy (TOF) Definition: Congenital heart defect with four characteristic features: Ventricular Septal Defect (VSD) Pulmonary Stenosis (RV outflow tract obstruction) Overriding Aorta (aorta arises from both ventricles) Right Ventricular Hypertrophy (secondary to pulmonary stenosis) Clinical Features: Cyanosis (blue baby syndrome), "tet spells" (paroxysmal hypercyanotic episodes, squatting to increase SVR), clubbing, poor growth, systolic murmur. Management: Surgical repair (usually in infancy) to close VSD and relieve RV outflow obstruction. Prostaglandin E1 to maintain PDA patency if severe cyanosis before surgery. Acute Pancarditis Etiology: Most commonly acute rheumatic fever. Can also be viral, bacterial, autoimmune. Clinical Features: Inflammation of all three layers of the heart: Pericarditis: Chest pain, pericardial rub. Myocarditis: Heart failure symptoms (dyspnea, fatigue), arrhythmias. Endocarditis: New or changing murmurs (especially mitral/aortic regurgitation). Fever, elevated inflammatory markers. Management: Treat underlying cause (e.g., antibiotics for GAS in ARF), anti-inflammatory drugs (NSAIDs, corticosteroids), supportive care for heart failure/arrhythmias. Wenckebach's Phenomenon Synonym for Second-Degree AV Block, Mobitz Type I. ECG: Progressive lengthening of the PR interval until a P wave fails to conduct (no QRS follows), then the cycle repeats. Clinical Significance: Often benign, usually asymptomatic, but may require pacemaker if symptomatic bradycardia occurs. Transesophageal Echocardiography (TEE) Definition: Echocardiography performed by inserting a probe into the esophagus, providing clearer images of the heart structures due to proximity. Indications: Better visualization of posterior structures (left atrium, mitral valve, aortic valve, descending aorta). Detection of LAA thrombus (before cardioversion for AF). Evaluation of prosthetic valve function. Diagnosis of endocarditis vegetations, abscesses. Assessment of aortic dissection. Intraoperative monitoring during cardiac surgery. Advantages: Higher resolution, less interference from lung/chest wall. Disadvantages: Invasive, requires sedation, potential for esophageal injury. Beta-Blockers Mechanism: Block beta-adrenergic receptors, reducing heart rate, contractility, and blood pressure. Examples: Metoprolol, carvedilol, bisoprolol, atenolol, propranolol. Indications: Hypertension, angina, post-MI, heart failure (with reduced EF), arrhythmias (rate control), anxiety, migraine prophylaxis. Side Effects: Bradycardia, hypotension, fatigue, bronchospasm (non-selective), erectile dysfunction. Contraindications: Severe bradycardia, high-degree AV block, uncontrolled asthma, cardiogenic shock. Serum Markers of Acute Myocardial Infarction (AMI) Cardiac Troponins (I and T): Most sensitive and specific. Rise within 3-12 hours, peak at 12-24 hours, remain elevated for 5-14 days. Creatine Kinase-MB (CK-MB): Less specific than troponins. Rises within 3-12 hours, peaks at 24 hours, normalizes within 48-72 hours. Useful for detecting re-infarction. Myoglobin: Early marker (rises within 1-4 hours), but not specific to cardiac muscle. Not routinely used for diagnosis. Pericarditis Definition: Inflammation of the pericardium. Etiology: Viral (most common), bacterial, autoimmune, uremia, post-MI (Dressler's), malignancy. Clinical Features: Sharp, pleuritic chest pain, often relieved by leaning forward, exacerbated by lying flat or inspiration. Pericardial friction rub (pathognomonic). Fever. ECG: Diffuse ST elevation (concave up), PR depression. Management: NSAIDs (ibuprofen, high dose), colchicine. Corticosteroids for refractory cases. Treat underlying cause. Complete Heart Block (CHB) Synonym for Third-Degree AV Block. ECG: Complete AV dissociation; no P waves conduct to ventricles. Atrial rhythm (P-P interval) and ventricular rhythm (R-R interval) are independent. Ventricular rate is typically slow ($ Clinical: Often symptomatic (syncope, dizziness, heart failure) due to severe bradycardia. Management: Permanent pacemaker. Left Ventricular Failure (LVF) Definition: Inability of the left ventricle to pump blood effectively to the systemic circulation, leading to reduced cardiac output and/or pulmonary congestion. Etiology: CAD, hypertension, valvular heart disease (aortic/mitral), cardiomyopathy. Clinical Features: Dyspnea (exertional, orthopnea, PND), cough, crackles, S3 gallop, pulmonary edema, fatigue. Management: Diuretics, ACEI/ARBs, beta-blockers, SGLT2 inhibitors, MRAs. Oxygen, nitrates for acute decompensation. Ventricular Ectopics (Premature Ventricular Contractions - PVCs) Definition: Premature electrical impulses originating from the ventricles. ECG: Wide, bizarre QRS complex, not preceded by a P wave, followed by a compensatory pause. Clinical: Often asymptomatic, or "skipped beats," palpitations. Usually benign, but frequent PVCs can lead to cardiomyopathy. Increased risk if underlying heart disease. Management: Usually not required if asymptomatic and no structural heart disease. Treat underlying causes (ischemia, electrolytes). Beta-blockers for symptomatic relief. DC Cardioversion Definition: Delivery of a synchronized electrical shock to the heart to terminate a tachyarrhythmia and restore sinus rhythm. Indications: Unstable tachyarrhythmias (AF, atrial flutter, VT with pulse, SVT) with signs of hemodynamic compromise (hypotension, altered mental status, shock, acute heart failure, ischemic chest pain). Elective cardioversion for stable, persistent AF. Procedure: Synchronized with the R wave to avoid inducing VF. Requires sedation. Contraindications: Digoxin toxicity, stable rhythms where chemical cardioversion is preferred. Medical Closure of Patent Ductus Arteriosus (PDA) Definition: Persistent communication between the aorta and pulmonary artery after birth. Medical Closure: Primarily in premature infants. Medication: Indomethacin or ibuprofen (NSAIDs). Mechanism: Inhibit prostaglandin synthesis, which is responsible for maintaining ductal patency. Indications: Symptomatic PDA (e.g., heart failure) in premature infants. Surgical/Catheter Closure: For older infants/children or when medical therapy fails. Anacrotic Pulse Definition: A pulse with a small additional notch or wave on the upstroke of the arterial pulse tracing. Clinical Significance: Often associated with severe aortic stenosis, indicating slow and delayed upstroke of the pulse. Also known as "pulsus parvus et tardus" (small and delayed pulse). Pulsus Paradoxus Definition: An abnormally large decrease in systolic blood pressure ($>10$ mmHg) during inspiration. Mechanism: During inspiration, increased venous return to the right heart causes the interventricular septum to bulge into the left ventricle, reducing LV filling and stroke volume. Clinical Significance: Highly suggestive of cardiac tamponade. Also seen in severe asthma, COPD, constrictive pericarditis. Hyperlipidemia Effects and Treatment Effects: Atherosclerosis (CAD, stroke, PAD), pancreatitis (severe hypertriglyceridemia). Treatment: Lifestyle: Diet (low saturated/trans fat, high fiber), exercise, weight loss, smoking cessation. Pharmacological: Statins: First-line for LDL reduction, primary/secondary prevention of ASCVD. Ezetimibe: Cholesterol absorption inhibitor. PCSK9 Inhibitors: Potent LDL reduction, for high-risk patients. Fibrates: Primarily for high triglycerides. Niacin: Raises HDL, lowers LDL/triglycerides (less used due to side effects). Omega-3 Fatty Acids: For severe hypertriglyceridemia. Angiotensin Receptor Blockers (ARBs) Mechanism: Block the binding of angiotensin II to its AT1 receptor, leading to vasodilation, decreased aldosterone secretion, and reduced cardiac remodeling. Examples: Valsartan, losartan, candesartan. Indications: Hypertension, heart failure, diabetic nephropathy, post-MI (especially if ACEI intolerant due to cough). Side Effects: Hypotension, hyperkalemia, renal dysfunction. Less cough/angioedema than ACEIs. Aortic Aneurysm Definition: Localized dilatation of the aorta, typically $>1.5$ times its normal diameter. Types: Thoracic Aortic Aneurysm (TAA): Occurs in the chest (ascending, arch, descending). Abdominal Aortic Aneurysm (AAA): Occurs in the abdomen, most commonly infrarenal. Etiology: Atherosclerosis (most common), genetic (Marfan, Ehlers-Danlos), hypertension, vasculitis, infection. Clinical Features & Signs: Often asymptomatic until rupture. AAA: May present with a palpable pulsatile abdominal mass (often infrarenal). Back or abdominal pain. Rupture: Sudden, severe abdominal/back pain, hypotension, pulsatile mass, syncope. Medical emergency. TAA: Compression symptoms: Chest/back pain, dyspnea, cough, hoarseness (due to recurrent laryngeal nerve compression), dysphagia. If involving aortic root, may cause aortic regurgitation (diastolic murmur). Rupture: Sudden, severe chest/back pain, shock. Diagnosis: Ultrasound (AAA screening/monitoring), CT angiography (CTA) or MRI (TAA, detailed assessment), echocardiography (proximal TAA). Management: Medical: Blood pressure control (beta-blockers), smoking cessation, lipid management. Regular surveillance imaging. Surgical/Endovascular: Indicated for symptomatic aneurysms, rapidly expanding aneurysms, or those reaching a critical size (e.g., AAA >5.5 cm, TAA >6.0 cm, depends on location and patient factors) to prevent rupture. Open repair: Surgical graft replacement. Endovascular Aneurysm Repair (EVAR/TEVAR): Minimally invasive stent-graft placement. Aortic Regurgitation (AR) Definition: Diastolic flow of blood from the aorta into the left ventricle due to incompetent aortic valve closure. Etiology: Acute: Infective endocarditis, aortic dissection, trauma. Chronic: Bicuspid aortic valve, rheumatic heart disease, Marfan syndrome, syphilis, hypertension, connective tissue diseases (e.g., ankylosing spondylitis). Clinical Features: Acute AR: Sudden onset of severe dyspnea, pulmonary edema, hypotension, cardiogenic shock. Requires urgent surgery. Chronic AR: Often asymptomatic for many years. Dyspnea on exertion, fatigue, palpitations (especially at night). Angina (due to increased myocardial oxygen demand and reduced diastolic coronary perfusion). Water-hammer (collapsing) pulse (Corrigan's pulse). Wide pulse pressure (high SBP, low DBP). Many peripheral signs: De Musset's sign (head bobbing), Muller's sign (uvular pulsation), Quincke's sign (capillary pulsations). Murmur: High-pitched, early diastolic decrescendo murmur, best heard at left sternal border (Erb's point) with patient leaning forward and exhaling. May have Austin Flint murmur. LV hypertrophy and dilation. Investigations: Echocardiography (confirmatory, assesses severity, LV function, aortic root). Management: Medical: Vasodilators (ACEI/ARBs) to reduce afterload, diuretics for heart failure symptoms. Careful BP control. Surgical: Aortic valve replacement (AVR) or repair for severe symptomatic AR, or asymptomatic severe AR with LV dysfunction (EF Complications: Left ventricular dysfunction, heart failure, endocarditis, aortic dissection (if root dilation). Calcium Channel Blockers (CCBs) Mechanism: Block calcium influx into vascular smooth muscle and myocardial cells, causing vasodilation and reduced cardiac contractility/heart rate. Types: Dihydropyridines: (e.g., amlodipine, nifedipine) Primarily vasodilators, less effect on HR. Used for hypertension, angina. Non-dihydropyridines: (e.g., verapamil, diltiazem) Affect heart rate and contractility more. Used for hypertension, angina, arrhythmias (rate control in AF/SVT). Indications: Hypertension, angina, arrhythmias, Raynaud's phenomenon. Side Effects: Hypotension, bradycardia (non-dihydropyridines), peripheral edema (dihydropyridines), headache, constipation (verapamil). Duckett Jones Criteria (Jones Criteria) Definition: Diagnostic criteria for Acute Rheumatic Fever (ARF). Major Criteria: Carditis, Polyarthritis, Chorea, Erythema Marginatum, Subcutaneous Nodules. Minor Criteria: Arthralgia, Fever, Elevated ESR or CRP, Prolonged PR interval. Diagnosis: Evidence of preceding Group A Streptococcal infection (e.g., positive throat culture, rapid strep test, elevated ASO titer) plus 2 Major OR 1 Major and 2 Minor criteria. Noninvasive Cardiac Imaging Echocardiography (Transthoracic & Transesophageal): Ultrasound of the heart, assesses structure, function, valves, pressures. Cardiac MRI: Detailed imaging of cardiac anatomy, function, tissue characterization (fibrosis, edema), viability. Gold standard for RV assessment. Cardiac CT: Coronary CT angiography (CTA) for CAD exclusion/diagnosis, calcium scoring. Assessment of great vessels, pericardium. Nuclear Cardiology (SPECT, PET): Myocardial perfusion imaging (stress tests) for ischemia, viability assessment. ECG (Electrocardiography): Basic electrical activity, rhythm, ischemia, hypertrophy. Rheumatic Chorea (Sydenham's Chorea) Definition: A neurological manifestation of acute rheumatic fever, characterized by involuntary, purposeless, jerky movements. Clinical Features: Affects limbs, face, and trunk. Often accompanied by emotional lability ("chorea insaniens"). Usually self-limiting but can be distressing. Management: Supportive care, sedatives (benzodiazepines), dopamine blockers (haloperidol) for severe cases. Digoxin Toxicity See "Treatment of Digitalis Toxicity" above. Apical Impulse Definition: The lowest and outermost point on the chest wall where the cardiac impulse can be palpated. Also known as the Point of Maximal Impulse (PMI). Normal Location: Fifth intercostal space, midclavicular line. Displacement: Lateral/Inferior displacement: Cardiomegaly (e.g., dilated cardiomyopathy, LV hypertrophy). Sustained/Heaving: LV hypertrophy. Diffuse: Dilated cardiomyopathy. Prevention and Management of Venous Thromboembolism (VTE) Includes: Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). Risk Factors: Virchow's Triad (venous stasis, endothelial injury, hypercoagulability). Surgery, immobility, cancer, trauma, OCPs, pregnancy, genetic thrombophilias. Prevention: Mechanical: Early ambulation, compression stockings, intermittent pneumatic compression (IPC). Pharmacological: Low molecular weight heparin (LMWH), unfractionated heparin (UFH), direct oral anticoagulants (DOACs) for high-risk patients. Management: Anticoagulation: Initial (LMWH/UFH/fondaparinux) followed by long-term (DOACs, warfarin) for at least 3-6 months. Thrombolysis: For massive PE with hemodynamic instability. IVC Filter: For patients with contraindications to anticoagulation or recurrent VTE despite adequate anticoagulation. Unstable Angina Definition: A form of Acute Coronary Syndrome (ACS) characterized by new onset angina, angina that is increasing in frequency/intensity, or angina occurring at rest. No elevation of cardiac biomarkers. Pathophysiology: Usually due to rupture of an atherosclerotic plaque with partial or transient occlusion of a coronary artery. Management: Similar to NSTEMI; antiplatelets (aspirin, P2Y12 inhibitors), anticoagulation (heparin), beta-blockers, nitrates, statins. Risk stratification and possible early coronary angiography. Constrictive Pericarditis Definition: A rare condition where the pericardium becomes thickened, fibrotic, and rigid, restricting diastolic filling of the ventricles. Etiology: Previous pericarditis (viral, bacterial, radiation), cardiac surgery, TB. Clinical Features: Symptoms of right heart failure (JVD, ascites, peripheral edema), Kussmaul's sign (paradoxical rise in JVP with inspiration), pericardial knock (early diastolic sound), pulsus paradoxus (less common than tamponade). Diagnosis: Echocardiography, CT/MRI (pericardial thickening), cardiac catheterization (equalization of diastolic pressures). Treatment: Pericardiectomy (surgical removal of the pericardium) is the definitive treatment. Diuretics for symptom relief. Angiotensin Converting Enzyme (ACE) Inhibitors Mechanism: Block the conversion of angiotensin I to angiotensin II, leading to vasodilation, decreased aldosterone secretion, and reduced cardiac remodeling. Examples: Enalapril, lisinopril, ramipril, captopril. Indications: Hypertension, heart failure, diabetic nephropathy, post-MI. Side Effects: Hypotension, hyperkalemia, renal dysfunction, dry cough, angioedema. Contraindications: Pregnancy, bilateral renal artery stenosis (relative), angioedema history. Prinzmetal Angina (Variant Angina) Definition: Chest pain caused by transient coronary artery spasm, leading to myocardial ischemia. Clinical Features: Often occurs at rest, typically in the early morning. Can be severe. ECG shows transient ST elevation during episodes. Risk Factors: Smoking. Diagnosis: Clinical history, ECG changes, sometimes provocative testing with ergonovine/acetylcholine. Treatment: Calcium channel blockers (first-line), nitrates. Avoid beta-blockers (can worsen spasm). Ventricular Septal Defects (VSDs) Definition: A hole in the interventricular septum, allowing blood to shunt between the left and right ventricles. Types: Perimembranous (most common), muscular, supracristal, AV canal type. Clinical Features: Small VSD: Often asymptomatic, loud holosystolic murmur at left lower sternal border. Large VSD: Symptoms of heart failure (dyspnea, fatigue, poor feeding, FTT) due to left-to-right shunt, pulmonary hypertension (Eisenmenger syndrome if irreversible). Management: Small VSD: Many close spontaneously. Large VSD: Medical management of heart failure (diuretics, digoxin, ACEI). Surgical closure or catheter device closure if symptomatic, pulmonary hypertension, or impending Eisenmenger. Cardiac Tamponade - Clinical Signs Definition: Compression of the heart due to rapid or large accumulation of fluid in the pericardial sac, impairing ventricular filling and reducing cardiac output. Beck's Triad: Hypotension: Due to reduced cardiac output. Muffled Heart Sounds: Fluid dampens sounds. Elevated Jugular Venous Pressure (JVP): Due to impaired right ventricular filling. Other Signs: Pulsus paradoxus, tachycardia, dyspnea, Kussmaul's sign (less common). Diagnosis: Echocardiography. Management: Urgent pericardiocentesis. Austin Flint Murmur Definition: A low-pitched, mid-diastolic or pre-systolic rumble heard at the apex. Clinical Significance: Associated with severe aortic regurgitation. Caused by the regurgitant aortic jet interfering with mitral valve opening or causing functional mitral stenosis. Distinction: No opening snap, unlike mitral stenosis. Collapsing Pulse (Water-Hammer Pulse) Definition: A strong, rapidly rising and falling arterial pulse. Clinical Significance: Characteristic of severe aortic regurgitation, due to large stroke volume and rapid diastolic runoff. Best appreciated by palpating the radial or brachial artery with the arm elevated. Antiarrhythmic Drugs Vaughan Williams Classification: Class I (Sodium Channel Blockers): Ia (e.g., procainamide, quinidine): Lengthen APD. Ib (e.g., lidocaine, mexiletine): Shorten APD. Ic (e.g., flecainide, propafenone): Minimal effect on APD. Used for VT, SVT, AF. Class II (Beta-Blockers): (e.g., metoprolol, propranolol) Decrease HR, slow AV conduction. Used for SVT, AF rate control, VT prevention. Class III (Potassium Channel Blockers): (e.g., amiodarone, sotalol, dronedarone, dofetilide) Prolong repolarization and refractory period. Used for AF, VT, VF. Class IV (Calcium Channel Blockers): (e.g., verapamil, diltiazem) Slow AV conduction, decrease HR. Used for SVT, AF rate control. Miscellaneous: Adenosine (SVT), Digoxin (AF rate control), Atropine (bradycardia). Treatment of Paroxysmal Supraventricular Tachycardia (PSVT) Definition: A rapid heart rhythm originating above the ventricles, with a regular narrow QRS complex. Acute Management: Vagal Maneuvers: Valsalva, carotid sinus massage, diving reflex. Adenosine (IV): First-line pharmacologic agent. Blocks AV node conduction. IV Beta-blockers or Calcium Channel Blockers (verapamil, diltiazem): If adenosine ineffective or contraindicated. DC Cardioversion: If hemodynamically unstable. Long-term Prevention: Catheter ablation (curative), beta-blockers, calcium channel blockers. Clinical Features of Marfan's Syndrome Definition: Autosomal dominant connective tissue disorder caused by a mutation in the FBN1 gene (fibrillin-1). Cardinal Features: Skeletal: Tall stature, arachnodactyly (long, slender fingers), joint hypermobility, pectus excavatum/carinatum, scoliosis. Ocular: Lens dislocation (ectopia lentis), myopia. Cardiovascular (most serious): Aortic root dilation, aortic regurgitation, aortic dissection, mitral valve prolapse. Management: Regular cardiovascular monitoring (echo), beta-blockers/ARBs to slow aortic dilation, surgical repair of aorta/valves if indicated.