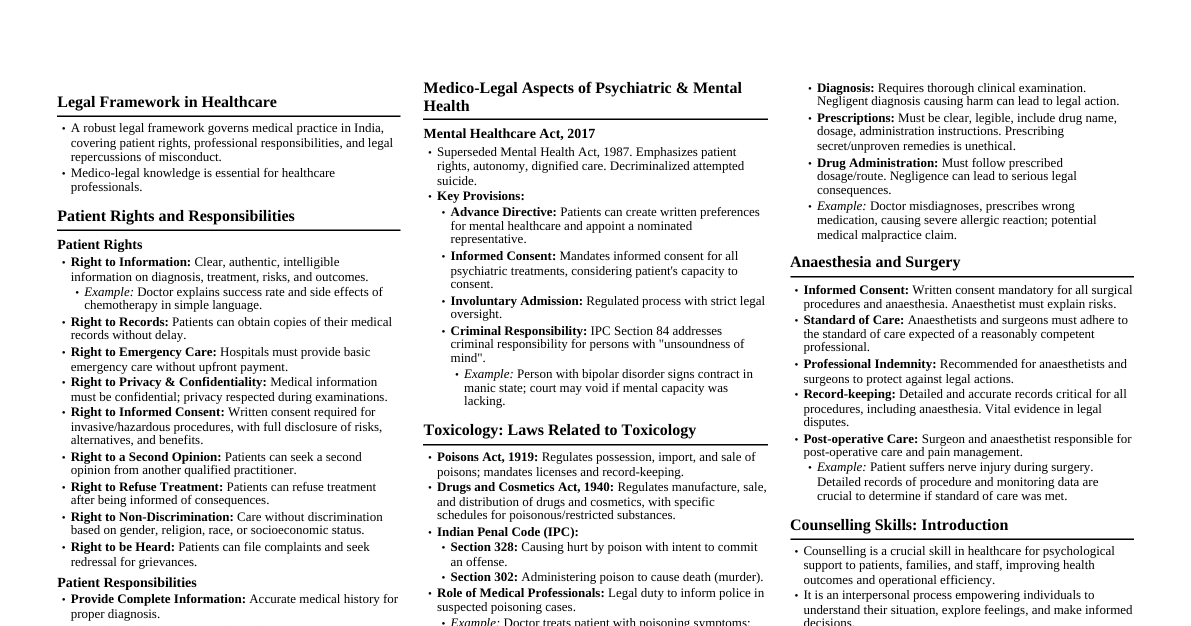
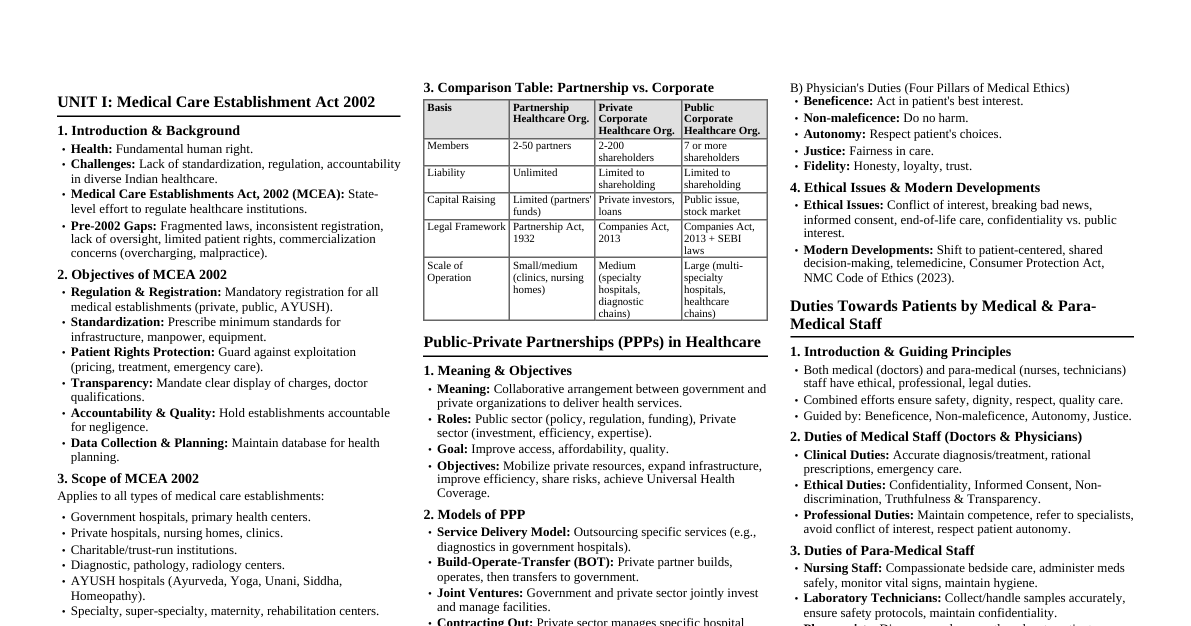
LEGAL FRAMEWORK: PATIENT RIGHTS AND RESPONSIBILITY 1. Introduction Patients are consumers of healthcare services, enjoying legal rights and protections. They also have responsibilities to ensure cooperation with healthcare providers. In India, patient rights are drawn from: Constitution of India (Right to Life – Article 21) Consumer Protection Act (CPA), 2019 Clinical Establishments Act, 2010 Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002 Charter of Patient Rights (2018) by MoHFW & NHRC 2. Legal Framework for Patient Rights A) Constitutional Rights Right to Life and Health (Article 21): Includes right to timely, adequate, and affordable healthcare. Right to Equality (Article 14): No discrimination in treatment. Right to Privacy (Article 21, Puttaswamy case 2017): Confidentiality of medical records. B) Statutory Rights Right to Information: Under RTI Act, 2005 and CPA, 2019. Patients can seek details about treatment, costs, and hospital policies. Right to Informed Consent: Patients must be informed about diagnosis, risks, benefits, alternatives before treatment. Right to Emergency Care: Parmanand Katara v. Union of India (1989) – Hospitals (public or private) cannot refuse emergency care. Right to Choose Provider and Treatment: Patients may select doctors, seek second opinion, and refuse treatment. Right to Dignity and Respect: Protection against inhuman or degrading treatment. Right to Confidentiality: Medical history, diagnosis, and records must be kept private. Right to Redressal: Patients can file complaints under CPA, 2019 for medical negligence, deficiency in service, or unfair trade practices. C) Charter of Patients' Rights (2018) Right to access healthcare. Right to non-discrimination. Right to informed consent. Right to privacy and confidentiality. Right to proper referral and transfer. Right to protection for participants in clinical trials. Right to take discharge/refuse treatment. Right to redressal. 3. Patient Responsibilities Provide Accurate Information: Share truthful details about medical history, allergies, lifestyle, and current illness. Compliance with Treatment: Follow doctor's advice, take medicines on time, and attend follow-up visits. Respect Healthcare Providers: Show courtesy to doctors, nurses, and staff; avoid violence or harassment against healthcare workers. Respect Hospital Rules: Follow admission, visiting hours, hygiene rules, and COVID-19 or infection protocols. Financial Responsibility: Pay bills and charges for treatment on time (unless covered under insurance or government schemes). Consideration for Other Patients: Maintain discipline; avoid causing inconvenience to fellow patients. Avoid Misuse of Rights: Do not demand unnecessary tests, medicines, or fraudulent insurance claims. 4. Legal Remedies for Patients Consumer Forums (CPA, 2019): Compensation for medical negligence or deficiency in service. Civil Courts: For damages. Criminal Law: IPC Sections 304A, 337, 338 for negligence causing death/injury. Regulatory Bodies: Medical Council of India (now NMC), State Medical Councils for professional misconduct. NHRC / State HRC: For human rights violations. MEDICAL MALPRACTICE 1. Introduction Professional negligence or misconduct by a doctor, nurse, paramedical staff, or hospital, leading to harm, injury, or death. Occurs when healthcare providers fail to meet the standard of care expected from a reasonably competent professional in similar circumstances. 2. Essential Elements of Medical Malpractice For a malpractice claim to be valid, four elements must be proved: Duty of Care: A doctor-patient relationship exists, creating a legal duty to provide treatment. Breach of Duty: Failure to provide care as per accepted medical standards (wrong diagnosis, improper treatment, surgical error, etc.). Causation: The breach directly caused injury or worsened the patient's condition. Damage: Patient suffered physical injury, mental trauma, disability, financial loss, or death. 3. Examples of Medical Malpractice in Hospitals Wrong diagnosis or delayed diagnosis. Surgical errors (wrong-site surgery, leaving instruments inside body). Medication errors (wrong drug/dose, allergy ignored). Negligence in monitoring patients (esp. ICU/emergency). Blood transfusion with mismatched blood group. Lack of informed consent before procedures. Failure to provide emergency care ( Parmanand Katara vs Union of India, 1989 ). Hospital-acquired infections due to poor hygiene. 4. Legal Framework in India A) Civil Liability Patients can claim compensation for damages under: Consumer Protection Act (CPA), 2019: Medical services = "service", patients are consumers. Tort Law: Negligence lawsuits in civil courts. B) Criminal Liability Under Indian Penal Code (IPC): Sec. 304A: Causing death by negligence. Sec. 337, 338: Causing hurt/grievous hurt by negligence. Doctors may face imprisonment + fine if gross negligence is proved. C) Professional/Disciplinary Liability National Medical Commission (NMC) / State Medical Councils can: Suspend or cancel medical license. Issue warnings for professional misconduct. 5. Landmark Cases Indian Medical Association vs V.P. Shantha (1995) – Medical services fall under CPA; patients can seek compensation for negligence. Jacob Mathew vs State of Punjab (2005) – Laid down distinction between civil negligence and criminal negligence. Criminal liability requires gross negligence. Kunal Saha Case (2013) – Supreme Court awarded ₹6.08 crore compensation (highest in Indian medical negligence cases) for wrongful treatment. 6. Defenses Available to Doctors/Hospitals No negligence: Injury was due to underlying disease, not treatment. Error of judgment: If taken with due care, not negligence. Contributory negligence: Patient's own negligence (not following treatment, hiding medical history). Emergency situation: Best efforts made in urgent life-threatening condition. Consent: Informed consent obtained from patient/guardian. 7. Consequences of Medical Malpractice For Patients: Injury, disability, trauma, loss of trust. For Hospitals/Doctors: Compensation, license suspension, imprisonment, loss of reputation. For Healthcare System: Rising defensive medicine, higher insurance premiums, mistrust. 8. Prevention of Medical Malpractice Strict adherence to medical protocols and SOPs. Proper documentation (case sheets, consent forms, discharge summaries). Effective communication with patients and families. Continuous medical education and training. Adoption of hospital accreditation standards (NABH, JCI). Medical indemnity insurance for doctors and hospitals. MEDICO LEGAL ASPECTS OF: IMPOTENCE, STERILITY, STERILIZATION AND ARTIFICIAL INSEMINATION 1. Impotence Meaning: Inability of a man to perform normal sexual intercourse (erectile dysfunction). Relevant in marriage, divorce, annulment, and criminal cases. Medico-Legal Aspects Matrimonial Issues: Under Hindu Marriage Act, 1955 and other personal laws, impotence (pre-existing and incurable) may be grounds for annulment of marriage. Criminal Cases: In rape cases, medical examination of the accused may be ordered to rule out impotence. Examination: Conducted only with court order or patient's consent; includes physical, psychological, and laboratory tests. Confidentiality: Results must be confidential; misuse may defame the individual. 2. Sterility Meaning: Inability of a person (male or female) to procreate (biological infertility). May be primary (never conceived) or secondary (inability after previous conception). Medico-Legal Aspects Marriage & Divorce: Sterility itself is not a ground for divorce, but if concealed before marriage, it may amount to fraud under marriage laws. Civil Cases: May lead to claims of mental cruelty, fraud, or compensation. Criminal Cases: If caused by negligent medical treatment, patient can sue for medical negligence. Examination: Done only with consent/court order. 3. Sterilization Meaning: Surgical procedure rendering a person permanently infertile (e.g., vasectomy, tubectomy). Medico-Legal Aspects Consent: Essential requirement. Must be informed, written, voluntary. For females, consent of the woman herself is mandatory (husband's consent not legally required, but often taken for social reasons). Medical Negligence: Failure of sterilization (e.g., pregnancy post-procedure) may lead to liability if due to negligence. State of Haryana vs Santra (2000) – Compensation awarded for failed sterilization. Criminal Liability: Performing sterilization without consent = assault or grievous hurt (IPC §§ 319–326). Public Health: Governed by family welfare programs; unethical coercion is illegal. 4. Artificial Insemination (AI) Types: AIH: Artificial insemination by husband's semen. AID: Artificial insemination by donor's semen. Medico-Legal Aspects Consent: Written consent of wife and husband is mandatory (to avoid future disputes). Legitimacy of Child: Under Section 112, Indian Evidence Act, child born by AID with husband's consent is presumed legitimate. Without consent, legitimacy may be challenged. Confidentiality: Donor identity must remain confidential. Inheritance & Succession: Legally, a child born by AI is considered equivalent to a natural-born child if done with consent. Ethical Concerns: Risk of consanguinity if donor identity is misused. Commercial exploitation of donors is prohibited. Regulation: Governed by Assisted Reproductive Technology (ART) Act, 2021 and Surrogacy (Regulation) Act, 2021 in India. 5. Summary Table (Impotence, Sterility, Sterilization, AI) Aspect Medico-Legal Concerns Impotence Grounds for annulment of marriage; examined in rape cases; requires consent & confidentiality Sterility Not direct ground for divorce but concealment = fraud; negligence claims possible Sterilization Consent mandatory; failure may lead to negligence claims ( Santra case ); coercion illegal Artificial Insemination Consent of both partners required; child legitimate if with consent; donor confidentiality; governed by ART Act, 2021 MEDICO LEGAL ASPECTS OF PSYCHIATRIC & MENTAL HEALTH 1. Introduction Psychiatry deals with diagnosis, treatment, and rehabilitation of mental illnesses. Patients with psychiatric disorders are often vulnerable, making legal protections essential. In India, the Mental Healthcare Act (MHCA), 2017 is the cornerstone legislation, aligned with UN conventions on human rights. 2. Important Medico-Legal Issues in Psychiatry A) Consent and Capacity A mentally ill patient's ability to give valid consent depends on capacity: Must understand the nature/consequences of treatment. If incapable $\rightarrow$ consent from nominated representative under MHCA, 2017. Involuntary admission allowed only under strict safeguards. B) Civil Responsibility Contracts: A contract signed by a person of “unsound mind" (as per Indian Contract Act, 1872, Sec. 12) is void. Marriage & Divorce: Mental illness can be grounds for annulment/divorce under Hindu Marriage Act, 1955 and other personal laws, if it makes cohabitation impossible. Testamentary (Will-making): Only valid if the person is of sound mind at the time. C) Criminal Responsibility Indian Penal Code, Sec. 84: “Nothing is an offence which is done by a person who, at the time of doing it, by reason of unsoundness of mind, is incapable of knowing the nature of the act or that it is wrong/contrary to law." Known as the McNaughten Rule (basis of insanity defense). Court orders psychiatric evaluation of accused if insanity is pleaded. D) Civil Commitment & Admission Voluntary Admission: By patient if mentally capable. Involuntary Admission: With consent of nominated representative + medical certification. Emergency Admission: If patient is a danger to self/others. Judicial review ensures rights are protected. E) Rights of Mentally Ill Patients (MHCA, 2017) Right to dignity, privacy, and confidentiality. Right to community living and not to be segregated. Right to access mental healthcare services. Right to advance directive – patient can pre-decide mode of treatment. Right to protection from cruel, inhuman, degrading treatment. F) Criminal Law Issues Rape, sexual exploitation, or abuse of mentally ill patients = serious offences with stricter punishments. Patients in mental hospitals are considered vulnerable groups, requiring protection. G) Forensic Psychiatry Assessment of mental state in legal contexts (crime, testamentary disputes, matrimonial cases). Psychiatrist may act as expert witness in court. 3. Common Medico-Legal Concerns in Psychiatric Practice False certification of insanity for criminal advantage. Overuse of restraint or ECT without consent $\rightarrow$ human rights violation. Negligence in suicide prevention within hospitals. Misuse of substances prescribed (controlled under NDPS Act, 1985). Confidentiality vs. Duty to warn (if patient poses risk to others). 4. Landmark Case Laws in India Sheela Barse vs Union of India (1983) – SC ordered humane treatment of mentally ill prisoners. Rupa Ashok Hurra vs Ashok Hurra (2002) – Severe mental illness recognized as valid ground for divorce. Accused under Sec. 84 IPC – Many cases (e.g., Surendra Mishra vs State of Jharkhand, 2011 ) clarified that insanity defense must be proven at the time of crime. 5. Summary Table (Psychiatry) Aspect Legal Provision / Concern Consent Valid only if patient is of sound mind; otherwise nominated representative (MHCA, 2017) Civil liability Unsound mind = contract void; affects marriage, divorce, and will-making Criminal liability IPC Sec. 84 - Insanity defense (McNaughten Rule) Patient rights MHCA, 2017 – dignity, confidentiality, advance directives, protection Admission Voluntary, involuntary, or emergency – with safeguards Doctor's liability Negligence in suicide prevention, overuse of restraint/ECT, breach of confidentiality TOXICOLOGY - LAWS RELATED TO TOXICOLOGY Toxicology has deep medico-legal importance because poisons, drugs, and chemicals are often linked with crime, suicide, homicide, accidents, drug abuse, and environmental hazards. The laws related to toxicology ensure safe handling, regulate use, and provide punishments for misuse. 1. Definition Toxicology is the branch of science that deals with the study of poisons, their sources, properties, effects, detection, and treatment, as well as their legal implications. Father of modern toxicology $\rightarrow$ Paracelsus ("All things are poison... the dose makes the poison"). 2. Scope of Toxicology Clinical Toxicology: Diagnosis & treatment of poisoning in patients. Forensic Toxicology: Detection of poisons in medico-legal cases (suicide, homicide, accidental poisoning). Environmental Toxicology: Effect of toxins on air, water, soil, and ecosystem. Occupational Toxicology: Hazards in industries (lead, mercury, asbestos, pesticides). Analytical Toxicology: Laboratory detection of toxic substances in biological materials. 3. Classification of Poisons A) Based on Origin Plant poisons – Opium, Dhatura, Aconite. Animal poisons – Snake venom, scorpion sting. Mineral poisons – Arsenic, Mercury, Lead. Synthetic/Chemical poisons – Cyanide, Organophosphorus insecticides. B) Based on Action Corrosives (acids, alkalis). Neurotoxins (alcohol, barbiturates, cocaine). Cardiac poisons (digitalis). Asphyxiants (carbon monoxide, cyanide). Food poisons (botulinum toxin, contaminated food). 4. Routes of Entry Ingestion (oral). Inhalation (gases, fumes). Injection (IV drug abuse, snake bite). Absorption through skin (pesticides). 5. General Clinical Features of Poisoning GI upset: nausea, vomiting, abdominal pain. Nervous system: convulsions, coma, delirium. Respiratory: difficulty breathing, cyanosis. Cardiovascular: arrhythmias, shock. Pupils: pinpoint (opiates, organophosphates), dilated (dhatura, atropine). 6. General Management of Poisoning Rescue & First Aid: Remove from source, airway support. Decontamination: Gastric lavage, activated charcoal, skin wash. Antidotes: Opioid $\rightarrow$ Naloxone. Organophosphates $\rightarrow$ Atropine, Pralidoxime. Cyanide $\rightarrow$ Nitrites + Thiosulphate. Iron $\rightarrow$ Desferrioxamine. Paracetamol $\rightarrow$ N-acetylcysteine. Supportive care: Fluids, oxygen, ICU monitoring. 7. Postmortem Findings in Poisoning Smell (e.g., bitter almond in cyanide, garlic in phosphorus). Corrosion in stomach/intestine. Organ congestion (liver, kidney, lungs). Preserved viscera for forensic analysis: Stomach + contents, small intestine + contents. Portion of liver, kidney, spleen. Blood, urine. 8. Medico-Legal Aspects of Toxicology Nature of poisoning: Suicide, homicide, accidental, occupational. Crime detection: Poisons used in murder (arsenic, cyanide). Drug abuse: NDPS Act, 1985 regulates narcotics/psychotropics. Industrial & environmental poisoning: Bhopal Gas Tragedy (1984) . Medical negligence: Wrong drug/overdose leading to poisoning $\rightarrow$ liability. Legal Acts: IPC (Sec. 284, 328, 304), Poisons Act 1919, NDPS Act 1985, Drugs & Cosmetics Act 1940, Food Safety Act 2006. 9. Landmark Cases K.M. Nanavati Case (1962) – Forensic evidence played role (though not poison-related, important for toxicology evidence use). State of Haryana vs Santra (2000) – Linked to medical negligence in sterilization, relevant when toxic drugs are involved. Bhopal Gas Tragedy Case (1984) – Led to Environment Protection Act, 1986. 10. Summary Table (Toxicology) Aspect Details Definition Study of poisons, effects, and legal issues Types Clinical, forensic, environmental, occupational Routes Ingestion, inhalation, injection, absorption Examples Plant (Dhatura), Mineral (Arsenic), Chemical (Cyanide) Management Decontamination, antidotes, supportive care Legal Acts IPC, Poisons Act, NDPS Act, Drugs & Cosmetics Act, FSSA Forensic role Sample preservation, expert witness in court Laws Related to Toxicology 1. Indian Penal Code (IPC), 1860 Sec. 284: Negligent conduct with poisonous substances. Sec. 299–304: Culpable homicide / murder by administering poison. Sec. 328: Causing hurt by means of poison (common in cases of drugging for robbery, sexual assault). Sec. 272–273: Adulteration of food or drinks with poisonous/unsafe substances. Sec. 511: Attempt to commit such offences. 2. Code of Criminal Procedure (CrPC), 1973 Provides procedure for collection, preservation, and forwarding of toxicological samples (blood, viscera, vomit, urine, etc.) for forensic analysis. Magistrate's inquest in cases of suspected poisoning deaths. 3. Indian Evidence Act, 1872 Expert opinion of Forensic Toxicologist/Medical Examiner is admissible as evidence (Sec. 45). Chain of custody and proper documentation is essential for toxicology reports to hold evidentiary value. 4. Drugs and Cosmetics Act, 1940 Regulates manufacture, storage, sale, and distribution of drugs and cosmetics. Prevents sale of spurious, adulterated, or misbranded drugs. Punishments include fines, imprisonment, and cancellation of license. 5. Narcotic Drugs and Psychotropic Substances (NDPS) Act, 1985 Most important law for toxicology related to drug abuse. Regulates possession, sale, transport, consumption, and trafficking of narcotic drugs (heroin, cocaine, opium, cannabis) and psychotropic substances (LSD, amphetamines, MDMA). Provides stringent punishment (10–20 years imprisonment, heavy fines). Allows rehabilitation measures for addicts. 6. Poisons Act, 1919 Regulates import, possession, and sale of poisons. Each state notifies certain poisons as restricted substances. Licensing system for sale of poisons. 7. Explosives Act, 1884 & Explosive Substances Act, 1908 Controls chemicals/toxic materials used for making explosives. Misuse for terrorism or criminal purposes punishable. 8. Factories Act, 1948 Ensures safety of workers exposed to toxic chemicals, gases, and dust. Provides for health measures, protective equipment, medical check-ups, and compensation. 9. Environment Protection Act, 1986 Provides for prevention and control of environmental pollution by toxic substances, pesticides, industrial effluents, and hazardous waste. Empowered after Bhopal Gas Tragedy (1984) . 10. Insecticides Act, 1968 Regulates manufacture, sale, transport, distribution, and use of insecticides/pesticides. Prevents poisoning due to misuse or accidental exposure. 11. Food Safety and Standards Act (FSSA), 2006 Regulates contamination of food and beverages with toxic substances. Food Safety and Standards Authority of India (FSSAI) monitors. Adulteration with toxic substances is punishable. 12. Medico-legal Procedures in Toxicology Postmortem examination in poisoning deaths. Viscera preservation (stomach, intestine, liver, spleen, kidney, blood, urine). Forensic Toxicology Lab Reports $\rightarrow$ submitted to court. Proper chain of custody must be maintained. 13. Landmark Case K. M. Nanavati vs State of Maharashtra (1962) – Highlighted forensic evidence value. Bhopal Gas Tragedy (1984) – Led to enactment of Environment Protection Act, 1986. 14. Summary Table (Laws Related to Toxicology) Law / Act Toxicology Relevance IPC, 1860 Poisoning crimes, negligence, food adulteration CrPC, 1973 Inquest, sample collection, toxicology reports Evidence Act, 1872 Expert opinion admissibility Drugs & Cosmetics Act, 1940 Drug safety and quality NDPS Act, 1985 Narcotics and psychotropic substances Poisons Act, 1919 Sale & regulation of poisons Factories Act, 1948 Worker safety against toxic exposure Environment Protection Act, 1986 Industrial toxins, pollution control Insecticides Act, 1968 Pesticide regulation FSSA, 2006 Food adulteration with toxins GIVING EVIDENCE IN POLICE INVESTIGATION 1. Introduction Evidence: Any statement, document, or material object presented to help establish facts in a case. Doctors, nurses, and paramedical staff often encounter medico-legal cases (MLC) such as accidents, assaults, rapes, poisonings, suicides, homicides. They are legally bound to assist the police and judiciary by providing evidence. 2. Types of Evidence Doctors Provide A) Oral Evidence Statement given in court or to police. As per Sec. 161 CrPC $\rightarrow$ police may record statement of any person (including doctor). In court, oral testimony must be under oath. B) Documentary Evidence Medico-Legal Case Reports (MLC reports). Wound certificates, postmortem reports, age certificates, sexual assault examination reports, toxicology reports. Hospital records – admission notes, discharge summary, consent forms. C) Material Evidence Viscera, clothing, bullets, foreign bodies, preserved samples handed over to police under chain of custody. 3. Legal Provisions Indian Evidence Act, 1872 Sec. 45: Expert opinion admissible (doctors = expert witnesses). Sec. 118: All persons competent to testify unless incapable of understanding questions. CrPC, 1973 Sec. 174: Inquest into suspicious deaths. Sec. 175: Police officer can summon doctor to assist. Sec. 176: Magistrate inquiry in custodial or suspicious death. IPC, 1860 Failure to provide information in medico-legal cases can attract liability under Sec. 176, 202 IPC. 4. Duties of Medical Professionals in Evidence Maintain accurate documentation: MLC register, injury reports, treatment notes. Preserve evidence properly: Sealed, labeled, handed to police with signature. Give impartial testimony: Doctor is a neutral expert, not a party. Confidentiality vs Legal Duty: Patient confidentiality may be breached if law requires (e.g., reporting gunshot wounds, poisoning, rape). Appear in court when summoned: Non-appearance may lead to contempt of court. 5. Procedure of Giving Evidence Police Investigation Stage: Doctor may be asked to give statement under Sec. 161 CrPC. Only signed medical reports with official seal should be handed over. Court Stage: Examination-in-chief: Lawyer/judge questions the doctor on findings. Cross-examination: Defense counsel tests accuracy and credibility. Re-examination: Clarification of disputed points. Oath: Doctor testifies under oath/affirmation. 6. Precautions While Giving Evidence Speak truthfully, clearly, and confidently. Base statements only on medical facts and observations, not assumptions. Avoid jargon – explain findings in layman's terms if court asks. Keep copies of all reports (as originals go to court/police). Maintain professional neutrality – don't favor prosecution or defense. ORGAN TRANSPLANTATION 1. Definition Surgical removal of an organ/tissue from one person (donor) and placing it into another (recipient) to replace a damaged/non-functional organ. Organs commonly transplanted: kidney, liver, heart, lung, pancreas, cornea, bone marrow, skin. 2. Types of Transplantation Autograft: Tissue transplanted within the same individual (e.g., skin graft). Isograft: Between identical twins. Allograft (Homograft): Between two genetically different humans (most common). Xenograft (Heterograft): Between humans and animals (experimental, e.g., pig heart valves). 3. Sources of Organs Living donors: Kidney, part of liver, bone marrow, cornea. Cadaver donors: Brain-dead patients (heart, liver, lungs, corneas, pancreas). Paired organ donation: Exchange between two families (kidney). 4. Legal Framework in India Transplantation of Human Organs and Tissues Act (THOTA), 1994 (amended 2011) Governs organ donation and transplantation in India. Key Provisions: Authorization: Donation only with written, informed consent of donor or next of kin (for cadaveric). Living Donors: Only near relatives (parents, children, siblings, spouse, grandparents). Unrelated donor $\rightarrow$ needs approval from Authorization Committee (to prevent commercial trade). Brain Death Certification: Must be certified by a panel of 4 doctors (neurologist/neurosurgeon compulsory). Ban on Commercial Trading: Sale/purchase of human organs is a punishable offence (imprisonment + fine). Hospitals: Must be registered as transplant centers. Punishment: Up to 10 years imprisonment + fine for illegal organ trade. 5. Ethical Issues Consent & Autonomy: Donation must be voluntary, informed, and free of coercion. Brain Death vs Cardiac Death: Legal recognition of brain death is crucial. Commercial Exploitation: Preventing “organ mafia" and poverty-driven exploitation. Allocation of Organs: Fair and transparent system (NOTTO in India manages). Religious & Cultural Concerns: Some communities may resist organ donation. 6. Medico-Legal Aspects Brain Death Declaration: Must follow THOTA, 1994 guidelines. Requires certification by a team of doctors. Living Donor Evaluation: Medical + psychological fitness must be ensured. Proof of relationship required. Illegal Transplantation: Both doctors and hospitals can be held liable. Cases of “kidney racket” highlight risks. Consent: Must be in writing and properly documented. Hospital Records: Proper registers of donors/recipients, approval forms, brain death certificates must be maintained. 7. Organizations in India NOTTO: National Organ and Tissue Transplant Organization (coordinates organ sharing & allocation). ROTTO: Regional Organ and Tissue Transplant Organization. SOTTO: State Organ and Tissue Transplant Organization. 8. Landmark Case Prafull Goradia vs Union of India (1997) – Supreme Court upheld constitutional validity of THOTA, 1994. 9. Advantages of Transplantation Life-saving (e.g., kidney, liver, heart transplants). Restores quality of life. Encourages medical research and advancements. 10. Challenges in India Shortage of donors (low awareness, cultural barriers). Illegal organ trade. Lack of infrastructure in smaller hospitals. Need for better awareness campaigns. EUTHANASIA (MERCY KILLING) 1. Definition Euthanasia: Deliberate act of ending a person's life to relieve them from incurable suffering. Also called “mercy killing”. Differs from assisted suicide, where a person takes their own life with medical help. 2. Types of Euthanasia A) Based on Method Active Euthanasia: Direct action to cause death (e.g., lethal injection). Passive Euthanasia: Withholding or withdrawing life support (e.g., stopping ventilator, not giving life-prolonging drugs). B) Based on Consent Voluntary: Patient requests euthanasia knowingly and willingly. Non-voluntary: Patient unable to give consent (coma, vegetative state) $\rightarrow$ decision by relatives/court. Involuntary: Against patient's wishes (equivalent to murder). 3. Ethical Aspects Arguments in Favor: Right to die with dignity. Relief from unbearable pain and suffering. Avoids unnecessary prolongation of life in terminal illness. Arguments Against: Sanctity of life – life is sacred, not to be taken away. Slippery slope – risk of misuse (killing elderly/disabled for convenience). Medical ethics – doctors' duty is to save life, not end it. 4. Legal Position in India Active euthanasia: Illegal (considered homicide under IPC). Passive euthanasia: Allowed by Supreme Court under strict safeguards. Landmark Cases Aruna Shanbaug Case (2011) Nurse in vegetative state for 42 years. SC allowed passive euthanasia (withdrawal of life support) under strict guidelines. Common Cause vs Union of India (2018) SC recognized Right to Die with Dignity under Article 21 (Right to Life). Legalized passive euthanasia and permitted living wills (advance directives). 5. Advance Directive / Living Will A written document where a person states in advance: Whether they want life-support in case of terminal illness/vegetative state. Nominated representative to decide on their behalf. Must be executed before a magistrate. 6. Medico-Legal Aspects Active euthanasia: Punishable under IPC §§ 302 (murder) / 304 (culpable homicide). Abetment of suicide: Punishable under IPC § 306. Doctors must follow Supreme Court guidelines strictly in passive euthanasia cases. Proper medical board review, judicial oversight, and documentation are mandatory before withdrawal of life support. 7. International Perspective Legal in some countries: Netherlands, Belgium, Luxembourg, Canada, Colombia, some U.S. states. Most countries (including India) only allow passive euthanasia with safeguards. 8. Summary Table (Euthanasia) Type Legal Status in India Example Active Euthanasia Illegal (murder) Giving lethal injection Passive Euthanasia Legal under SC rulings (2011, 2018) Withdrawing ventilator in vegetative state Voluntary Allowed only in passive form Patient's living will Non-voluntary Allowed under court supervision Comatose patient decision Involuntary Illegal Killing against wishes DIAGNOSIS, PRESCRIPTIONS AND ADMINISTRATION OF DRUGS 1. Diagnosis Definition: Process of identifying a disease or condition based on patient history, clinical examination, investigations, and differential analysis. Legal and Ethical Aspects Duty of Care: A doctor is expected to exercise reasonable skill while diagnosing. Negligence arises if: Wrong diagnosis due to carelessness. Failure to order necessary tests. Ignoring patient's symptoms. Bolam Test (UK case law, also followed in India): A doctor is not negligent if they act in accordance with a practice accepted as proper by a responsible body of medical professionals. Medico-Legal Importance Incorrect or delayed diagnosis may lead to liability under tort (negligence) , Consumer Protection Act , or even criminal law if grossly negligent. Proper documentation of case history and diagnostic reasoning protects doctors. 2. Prescriptions Definition: A prescription is a written order by a registered medical practitioner directing the use of a specific drug/treatment for a patient. Essential Parts of a Valid Prescription Patient's name, age, sex, address. Date of prescription. Symbol "Rx” (Recipe: “Take thou”). Name of the drug (preferably generic, as per Indian Medical Council Regulations). Dose, route, frequency, and duration. Instructions (before/after meals, warnings). Prescriber's name, signature, registration number. Legal and Ethical Aspects Only registered medical practitioners (RMPs) can prescribe. Generic drugs must be prescribed, unless specific reasons justify branded drugs. Narcotics & psychotropics: require special prescription and records under NDPS Act, 1985. Prescription errors (wrong drug, wrong dose, illegible writing) may cause negligence liability. Issuing prescriptions without examining the patient (online/phone without proper telemedicine guidelines) is illegal/unethical. 3. Administration of Drugs Definition: Process of giving a drug to the patient by appropriate route (oral, injection, infusion, topical, etc.). Rights of Drug Administration (the “7 Rs" rule) Right patient Right drug Right dose Right route Right time Right documentation Right to refuse (patient autonomy) Legal and Ethical Aspects Drugs must be administered by qualified personnel (nurse, doctor, pharmacist as per law). Wrong route/dose/timing leading to harm = negligence. Informed consent is needed for high-risk drugs (chemotherapy, anesthesia, narcotics). Adverse Drug Reactions (ADRs) should be reported under Pharmacovigilance Programme of India (PvPI). Narcotic drug administration must follow NDPS Act and hospital SOPs. 4. Medico-Legal Liabilities Civil Liability (Compensation): Wrong diagnosis/prescription/administration causing injury. Criminal Liability: Gross negligence causing death (IPC § 304A). Professional Misconduct: Prescribing without examination. Endorsing brand drugs for commercial gain. Prescribing banned drugs. Not maintaining prescription records. 5. Safeguards for Doctors & Hospitals Maintain complete patient records (diagnosis process, prescriptions, administration chart). Prescribe in legible handwriting (or computerized). Follow standard treatment guidelines. Obtain informed consent when necessary. Train staff in safe drug administration practices. Follow WHO Surgical Safety Checklist. ANAESTHESIA AND SURGERY 1. Anaesthesia Definition: Administration of drugs to induce a loss of sensation or consciousness to permit surgery or painful procedures. Types General Anaesthesia: Complete unconsciousness. Regional Anaesthesia: Blocks sensation in a large area (spinal, epidural, nerve block). Local Anaesthesia: Numbness in a small area. Sedation: Patient relaxed but not fully unconscious. Legal & Ethical Aspects Informed Consent: Must include type of anaesthesia, risks (e.g., cardiac arrest, anaphylaxis, awareness under GA). Pre-Anaesthetic Check-Up (PAC): Mandatory – includes history (allergies, comorbidities), investigations, and risk grading (ASA classification). Competence: Only qualified anaesthesiologists can administer GA or regional blocks. Monitoring: Continuous monitoring of vitals (pulse, BP, oxygen saturation, ECG). Record Keeping: Anaesthesia notes, drug doses, complications, and monitoring charts must be documented. Errors Leading to Liability: Wrong drug, overdose, inadequate monitoring, failure to resuscitate. 2. Surgery Definition: Operative manual and instrumental techniques performed to treat disease, injury, or deformity. Legal & Ethical Aspects Informed Consent: Must include: diagnosis, procedure, risks, complications, alternatives, prognosis. Consent must be specific to the procedure (general consent is insufficient). In case of minors/unconscious patients $\rightarrow$ consent from guardian/legal representative. Emergency exceptions: Life-saving surgery can be performed without consent. Duty of Care: Surgeon must exercise reasonable degree of skill and diligence. Mistakes due to gross negligence (leaving instruments inside, operating wrong site) $\rightarrow$ liability. 3. Pre-Operative Care Risk assessment, investigations, anaesthetic clearance. 4. Intra-Operative Care Maintaining sterile technique. Avoiding wrong site/wrong patient surgery (WHO Surgical Safety Checklist). 5. Post-Operative Care Pain management, infection prevention, monitoring complications. Failure to provide post-op care = negligence. 3. Medico-Legal Liabilities Civil Liability: Compensation claims under negligence/Consumer Protection Act. Criminal Liability: If gross negligence causes death (IPC § 304A). Professional Misconduct: Operating without consent. Performing unnecessary surgery for profit. Delegating surgery to unqualified persons. 4. Special Situations Emergency Surgery: Can proceed without consent if delay endangers life. Sterilization & Abortion Surgeries: Strict compliance with laws (MTP Act, Family Welfare guidelines). Cosmetic Surgery: Requires detailed consent, since results may be subjective. High-Risk Surgeries: Must explain possibility of death/disability. 5. Safeguards for Anaesthetists & Surgeons Take informed and written consent (preferably video consent in sensitive cases). Conduct pre-operative evaluation and document fitness. Maintain detailed operative notes and anaesthesia charts. Use standard instruments and sterilization practices. Ensure trained staff and resuscitation equipment availability. Follow WHO Surgical Safety Checklist.