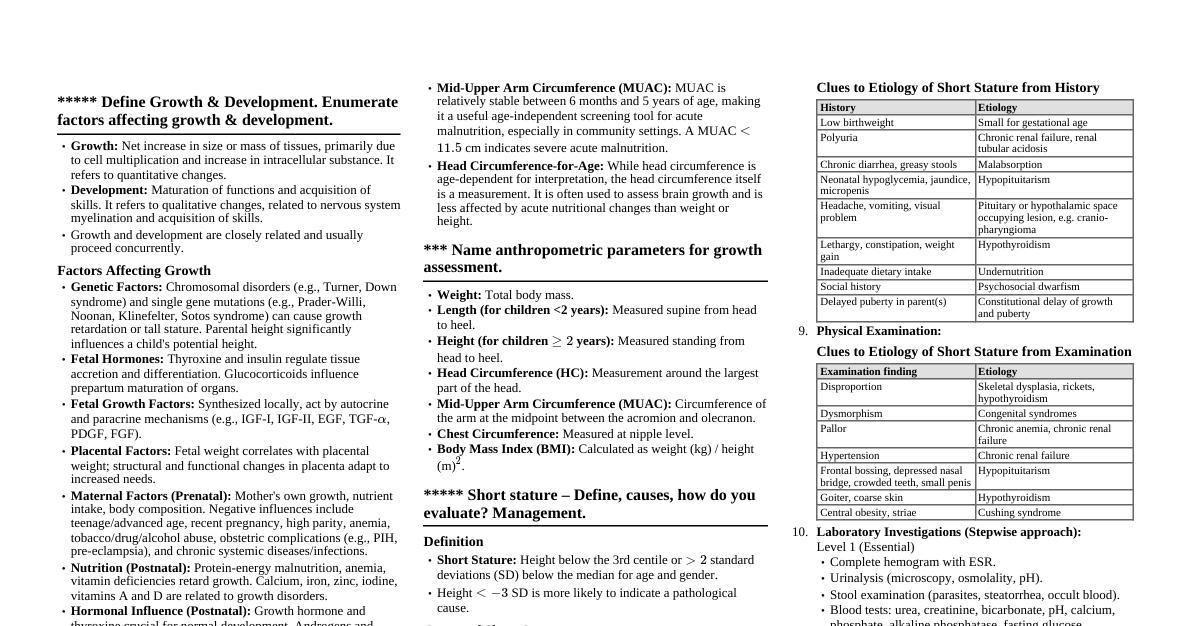
Growth & Development: Definitions Growth: Quantitative increase in size/mass due to cell multiplication and intracellular substance increase. Development: Qualitative maturation of functions, nervous system, and acquisition of skills. Factors Affecting Growth & Development Factors Affecting Fetal Growth Genetic: Parental traits, sex. Fetal Hormones: Thyroxine, insulin, glucocorticoids. Fetal Growth Factors: IGF-I, IGF-II, EGF, TGF-$\alpha$, PDGF, FGF, NGF. Placental Factors: Structural/functional integrity. Maternal Factors: Nutrition, age, parity, health status (anemia, tobacco/alcohol, chronic diseases, infections, pre-eclampsia). Factors Affecting Postnatal Growth & Development Genetic: Chromosomal disorders (Turner, Down), gene mutations (Prader-Willi, Noonan). Nutrition: Breastfeeding, complementary feeding, malnutrition, vitamin deficiencies. Hormonal: Growth hormone, thyroxine, androgens, estrogens. Intrauterine Growth Restriction (IUGR): Risk for postnatal malnutrition. Environmental: Socioeconomic status, housing, hygiene, infections. Psychosocial: Nurturing environment, emotional stimulation, maternal depression, institutionalization. Sensory Inputs: Vision, hearing. Education: Maternal education. Anthropometric Parameters for Growth Assessment Weight: Overall nutritional status, acute changes. Length/Height: Linear growth, chronic malnutrition (stunting). Head Circumference (HC): Brain growth, especially 0-3 years. Body Mass Index (BMI): Weight/height proportionality ($\text{kg/m}^2$). Mid Upper Arm Circumference (MUAC): Acute malnutrition (6 months - 5 years). Weight-for-Length/Height: Wasting (acute malnutrition). Length/Height-for-Age: Stunting (chronic malnutrition). Weight-for-Age: General growth indicator. Age Independent Anthropometric Indices Useful when age is unknown. Weight-for-height: Assesses acute malnutrition (wasting). MUAC: Screens for acute malnutrition; relatively stable 6 months to 5 years. Short Stature: Definition, Causes, Evaluation, Management Definition Height $ 2\text{ SD}$ below mean for age/gender. Causes Normal Variants: Familial Short Stature: Normal growth velocity, normal bone age, target height. Constitutional Growth Delay: Decelerated growth, delayed puberty, delayed bone age, normal final height. Pathological Causes: Nutritional: Undernutrition, chronic systemic illness (renal, GI, cardiac). Endocrine: Growth Hormone Deficiency (GHD), Hypothyroidism, Cushing syndrome. Skeletal Dysplasias: Achondroplasia, spondyloepiphyseal dysplasia (disproportionate). Genetic Syndromes: Turner, Down, Prader-Willi, Russell-Silver. IUGR/SGA: Failure of catch-up growth. Psychosocial Dwarfism: Emotional deprivation. Miscellaneous: Corticosteroid use, renal tubular acidosis. Evaluation History: Birth, family (parental height, puberty), feeding, chronic illness, development, psychosocial. Physical Exam: Accurate anthropometry (plot on charts), growth velocity, body proportions (US:LS ratio, arm span), Tanner staging, dysmorphic features. Investigations: Bone age (X-ray hand/wrist), CBC, ESR, TFTs, IGF-1, IGFBP-3, Celiac serology, renal function, karyotype (for girls), genetic testing. Management Counseling, nutritional rehabilitation. Treatment of underlying cause: GH therapy (GHD, Turner, SGA), thyroid replacement (hypothyroidism), chronic illness management. Regular monitoring, psychological support. Laws of Growth Continuous and orderly, but not constant. Rapid during fetal life, infancy, and puberty; slowed in mid-childhood. Cephalocaudal and distal-to-proximal progression. Different tissues grow at different rates (brain, gonadal, lymphoid). Common Patterns of Development Continuous and orderly process. Depends on nervous system maturation. Sequence is consistent: babbling before words, sitting before standing. Cephalocaudal and proximodistal progression. Mass activity replaced by specific actions. Primitive reflexes must disappear for higher skills. Growth Charts Graphical tools for plotting anthropometric measurements against age/gender. Purpose: Identify abnormal growth (FTT, obesity, short stature), monitor velocity, evaluate interventions, screen for health problems. Components: Percentile curves (3rd-97th), Z-scores ($\text{SD}$ from mean), separate charts for boys/girls, age groups (0-5, 5-19 yr). Interpretation: Normal (tracking percentile), concerning (crossing percentiles, below 3rd/above 97th). Correct for prematurity (until 2 yr). Standards: WHO Growth Standards (0-5 yr), WHO Reference Data (5-19 yr). Microcephaly: Definition, Causes, Management Definition Occipitofrontal circumference (HC) $>2\text{ SD}$ below mean for age/sex. Primary (congenital) or Secondary (acquired). Causes Genetic: Isolated, syndromic (Trisomies, William, Cri-du-chat, Seckel). Prenatal: Infections (TORCH, Zika). Teratogens (alcohol, drugs). Maternal conditions (malnutrition, PKU). Structural malformations (lissencephaly). Perinatal: HIE, hyperbilirubinemia, intracranial hemorrhage. Postnatal: Severe malnutrition, hypothyroidism, infections (meningitis), TBI, metabolic disorders. Management No specific cure. Symptomatic and supportive care: Early intervention (PT, OT, speech), management of associated conditions (seizures, spasticity), nutritional support. Genetic counseling, regular monitoring. Macrocephaly: Definition, Causes Definition Occipitofrontal circumference (HC) $>2\text{ SD}$ above mean for age/sex. Causes Benign Familial Macrocephaly: Inherited, normal development. Hydrocephalus: Excess CSF (congenital/acquired). Megalencephaly: Increased brain tissue (Sotos, Fragile X, NF1, metabolic disorders). Subdural Collections: Benign external hydrocephalus, chronic subdural hematoma. Intracranial Space-Occupying Lesions: Tumors, cysts. Vascular Malformations: AVMs. Increased Bony Compartment: Achondroplasia, osteopetrosis. Developmental Milestones Key Gross Motor Developmental Milestones Age Milestone 3 mo Neck holding 5 mo Rolls over 6 mo Sits in tripod fashion 8 mo Sits without support 9 mo Stands holding on 12 mo Creeps well; walks but falls; stands without support 15 mo Walks alone; creeps upstairs 18 mo Runs; explores drawers 2 yr Walks up and downstairs (2 feet/step); jumps 3 yr Rides tricycle; alternate feet going upstairs 4 yr Hops on one foot; alternate feet going downstairs Key Fine Motor Developmental Milestones Age Milestone 4 mo Bidextrous reach 6 mo Unidextrous reach; transfers objects 9 mo Immature pincer grasp; probes with forefinger 12 mo Pincer grasp mature 15 mo Imitates scribbling; tower of 2 blocks 18 mo Scribbles; tower of 3 blocks 2 yr Tower of 6 blocks; vertical and circular stroke 3 yr Tower of 9 blocks; copies circle 4 yr Copies cross; bridge with blocks 5 yr Copies triangle; gate with blocks Key Social and Adaptive Milestones Age Milestone 2 mo Social smile 3 mo Recognizes mother; anticipates feeds 6 mo Recognizes strangers, stranger anxiety 9 mo Waves "bye bye" 12 mo Comes when called; plays simple ball game 15 mo Jargon 18 mo Copies parents in task 2 yr Asks for food, drink, toilet; pulls people to show toys 3 yr Shares toys; knows full name and gender 4 yr Plays cooperatively; goes to toilet alone 5 yr Helps in household tasks, dresses and undresses Key Language Milestones Age Milestone 1 mo Alerts to sound 3 mo Coos (musical vowel sounds) 4 mo Laugh loud 6 mo Monosyllables (ba, da, pa), ah-goo sounds 9 mo Bisyllables (mama, baba, dada) 12 mo 1-2 words with meaning 18 mo 8-10 word vocabulary 2 yr 2-3 word sentences, uses pronouns "I", "me", "you" 3 yr Asks questions; knows full name and gender 4 yr Says song or poem; tells stories 5 yr Asks meaning of words Global Developmental Delay (GDD) Definition: Significant delay ($>2\text{ SD}$ below mean or DQ $ Significance: Provisional diagnosis to initiate early intervention. Often precedes intellectual disability diagnosis. Breath-Holding Spells & Treatment Definition Involuntary, non-epileptic events of apnea, usually provoked by emotional upset/pain, leading to cyanosis/pallor, sometimes brief loss of consciousness. Clinical Features Age 6 months - 6 years, peaks 18-36 months. Precipitated by frustration, fear, pain. Sequence: Cry $\rightarrow$ exhale $\rightarrow$ apnea $\rightarrow$ cyanosis/pallor $\rightarrow$ limp/brief convulsions $\rightarrow$ rapid recovery. Types: Cyanotic (most common), Pallid. Self-limited, often associated with iron deficiency anemia. Management Reassurance & Education: Involuntary, harmless. Behavioral: Avoid triggers, distraction, consistency, safety during spells. Iron Supplementation: If iron deficiency present. Pharmacological (rare): Atropine for severe pallid spells. Attention Deficit Hyperactivity Disorder (ADHD) Definition Neurodevelopmental disorder with persistent pattern of inattention and/or hyperactivity-impulsivity, interfering with functioning, present before 12 years in $\ge 2$ settings. Clinical Features (DSM-5) Predominantly Inattentive Presentation: $\ge 6$ symptoms of inattention (careless mistakes, difficulty sustaining attention, doesn't listen, fails to finish tasks, disorganized, avoids mental effort, loses things, easily distracted, forgetful). Predominantly Hyperactive-Impulsive Presentation: $\ge 6$ symptoms of hyperactivity (fidgets, leaves seat, runs/climbs, unable to play quietly, "on the go," talks excessively) and/or impulsivity (blurts answers, difficulty waiting, interrupts). Combined Presentation: Meets criteria for both. Management Multimodal: Psychoeducation, behavioral therapy (parent training, school interventions, social skills), educational interventions (IEPs). Pharmacotherapy: Stimulants (Methylphenidate, Amphetamine salts): First-line for school-aged. Non-stimulants (Atomoxetine, Guanfacine, Clonidine): Alternatives or adjuncts. Lifestyle, address co-occurring conditions, ongoing monitoring. Pica Definition Persistent ingestion of non-nutritive, non-food substances for $\ge 1$ month, inappropriate for developmental level. Common Substances Dirt, clay, hair, paint chips, ice, paper, cloth. Associations & Risks Developmental delay, intellectual disability, ASD. Psychosocial stress, neglect. Nutritional deficiencies (iron, zinc). Risks: Poisoning (lead), infections (parasites), GI problems (obstruction, perforation), dental injury. Management Assessment (history, developmental level, psychosocial, medical eval: CBC, lead, stool O&P). Treat underlying conditions (iron, deworming, chelation). Behavioral interventions (environmental modification, supervision, positive reinforcement). Psychosocial support. Thumb Sucking Description Common self-soothing behavior in infants/young children. Natural reflex, often starts in utero. Normal Development Most infants/toddlers do it. Peaks 18-21 months. Spontaneously stops by 4-5 years. Reasons Self-soothing, comfort, anxiety, boredom, hunger. Potential Problems (if persistent/vigorous past 4-5 years) Dental issues (malocclusion, open bite, buck teeth). Speech problems, skin problems, social stigma. Management Under 4 years: No intervention, normal. Preschoolers (4-6 years): Ignore, identify triggers, gentle reminders, positive reinforcement, provide alternatives, dental consultation. Older children/persistent: Child's motivation crucial, explain consequences, physical barriers (nail polish, dental appliances - last resort), counseling. Avoid punishment. Red Flag Signs & Clinical Features of Autism Spectrum Disorder (ASD) Definition Neurodevelopmental condition with persistent deficits in social communication/interaction AND restricted, repetitive patterns of behavior/interests. Present from early childhood, impairs functioning. Red Flag Signs (Early Indicators) By 6 months: No big smiles/joyful expressions. By 9 months: No back-and-forth sharing (sounds, smiles, expressions). By 12 months: No babbling, no back-and-forth gestures (pointing, showing), no response to name. By 16 months: No single words. By 24 months: No meaningful two-word phrases. At Any Age: Loss of previously acquired speech/social skills, avoids eye contact, prefers to be alone, difficulty understanding feelings, delayed language, echolalia, unrelated answers, upset by minor changes, obsessive interests, hand flapping/rocking, unusual sensory reactions. Clinical Features (DSM-5) 1. Persistent Deficits in Social Communication & Social Interaction (across multiple contexts) Deficits in social-emotional reciprocity (abnormal social approach, reduced sharing of interests/emotions, failure to initiate/respond to social interaction). Deficits in nonverbal communicative behaviors (poorly integrated verbal/nonverbal, abnormal eye contact/body language, deficits in gestures, lack of facial expressions). Deficits in developing, maintaining, and understanding relationships (difficulties adjusting behavior to social context, sharing imaginative play, making friends, absence of interest in peers). 2. Restricted, Repetitive Patterns of Behavior, Interests, or Activities (at least two) Stereotyped or repetitive motor movements, use of objects, or speech (e.g., motor stereotypies, lining up toys, echolalia). Insistence on sameness, inflexible adherence to routines, or ritualized patterns (e.g., distress at small changes, rigid thinking, greeting rituals). Highly restricted, fixated interests abnormal in intensity/focus (e.g., preoccupation with unusual objects, perseverative interests). Hyper- or hyporeactivity to sensory input or unusual interests in sensory aspects (e.g., indifference to pain, adverse response to sounds/textures, excessive smelling, visual fascination). Asymmetric Tonic Neck Reflex (ATNR) Definition: Primitive reflex (fencer's pose) present at birth, typically integrates by 4-6 months. Elicitation: Head turned to one side $\rightarrow$ arm/leg on same side extend, opposite arm/leg flex. Purpose: Early unilateral movements, hand-eye coordination, prevents early rolling. Clinical Significance: Persistence beyond 6 months: Abnormal, suggests neurological dysfunction (e.g., cerebral palsy). Obligatory ATNR: Always pathological. Absence in newborn: Indicates neurological problems. Impact of Persistent ATNR: Interferes with symmetrical movements, midline activities, hand-eye coordination, crawling, walking. Notes on Behavioral Disorders a) Temper Tantrums Definition: Intense emotional outbursts (crying, screaming, hitting) in young children, due to frustration, lack of control, fatigue, or attention-seeking. Age: Common 18 months - 3 years, subsides by 4-5 years. Management: Prevention: Avoid triggers, offer choices, distraction, teach communication. During: Stay calm, ensure safety, ignore behavior, "time-out" (for older toddlers). After: Reconnect, discuss, praise positive behavior. Seek help if frequent, prolonged, aggressive, self-injurious, or beyond age 5-6. b) Enuresis Definition: Repeated involuntary/intentional urination (bed/clothes), $\ge 2 \text{x/week}$ for $\ge 3$ months, in child $\ge 5$ years. Types: Nocturnal, Diurnal, Mixed; Primary (never dry), Secondary (relapse after 6 months dry). Causes: Delayed bladder maturation, genetic, increased nighttime urine, small bladder capacity, deep sleep, constipation, stress, medical conditions (UTI, diabetes). Management: Behavioral (First-line): Reassurance, fluid restriction, scheduled voiding, motivational therapy, enuresis alarm. Pharmacological (Second-line): Desmopressin (DDAVP), Imipramine. Address underlying issues (constipation, stress). c) Encopresis Definition: Repeated involuntary/intentional passage of feces into inappropriate places, $\ge 1 \text{x/month}$ for $\ge 3$ months, in child $\ge 4$ years. Types: With constipation/overflow incontinence (most common), Without constipation. Causes: Chronic constipation (leading to impaction, reduced sensation), dietary factors, psychological factors (stress, anxiety), developmental delay. Management: Disimpaction: Oral laxatives/enemas to clear impacted stool. Maintenance: Daily laxatives, increased fluid/fiber. Behavioral: Scheduled toilet sitting, positive reinforcement, education. Psychological Support: Address underlying emotional issues. Avoid punishment. Long-term follow-up needed.