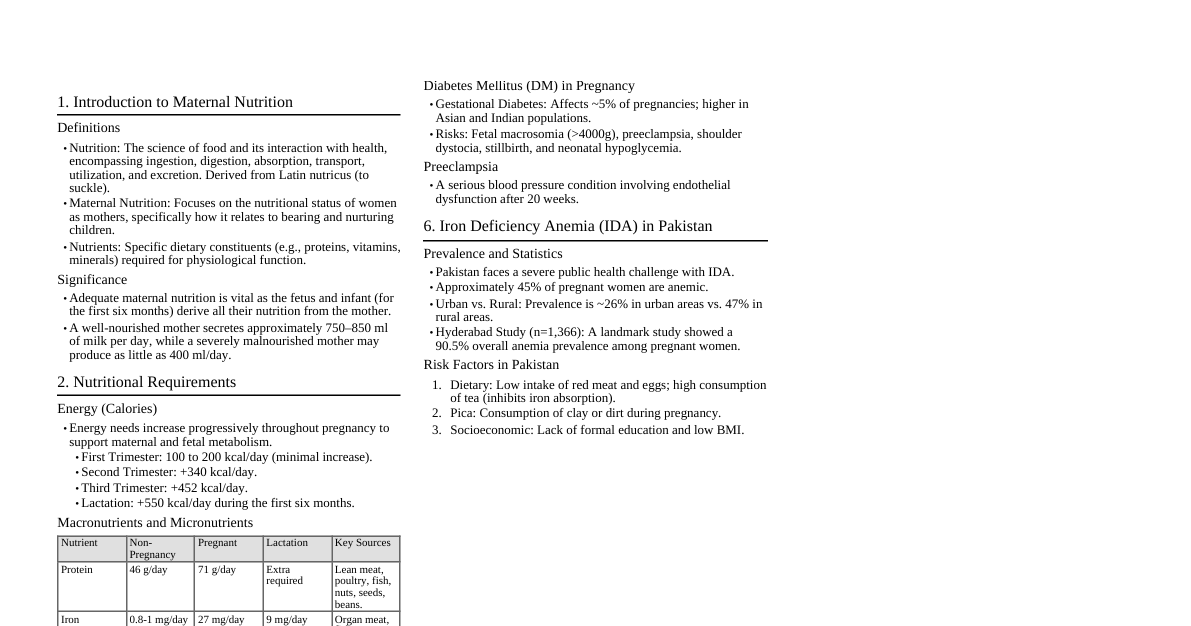
### Introduction to Maternal and Child Health Nursing (MCHN) MCHN focuses on nursing care for pregnant women, mothers, and children from birth to adolescence. It's crucial for population health, reducing mortality, and achieving sustainable health goals. ### Goals & Philosophies of MCHN - **Primary Goal:** Promotion and maintenance of optimal family health. - **Scope:** Extends from preconception to menopause. - **Approach:** Family-centered care is the preferred focus. ### Global Health Goals (MCH Focus) These goals align with Sustainable Development Goals (SDGs) to reduce mortality rates by 2030. - End poverty & hunger - Universal primary education - Promote gender equality & empower women - Reduce child mortality - Improve maternal health - Combat HIV/AIDS, malaria, & other diseases - Ensure environmental sustainability - Develop global partnerships ### Maternal Health Refers to the health of women during pregnancy, childbirth, and the postnatal period. Each stage should be a positive experience. #### Maternal Mortality Ratio (MMR) - **Definition:** Number of women who die due to pregnancy-related causes per 100,000 live births in a given period (usually one year). - **Reflection:** Quality of maternal healthcare, access to antenatal, delivery, and postnatal services, and overall health system strength. - **Formula:** $$ \text{MMR} = \frac{\text{Number of maternal deaths}}{\text{Number of live births}} \times 100,000 $$ - *Clue:* Multiplied by 100,000 for easier comparison and public health analysis (since maternal deaths are less frequent). - **Important Terms:** - **Maternal Death:** Death of a woman while pregnant or within 42 days of termination of pregnancy, from causes related to pregnancy or its management (not accidental/incidental causes). - **Live Birth:** Baby shows any sign of life after birth (breathing, heartbeat, movement), even if the baby dies later. - **Common Direct Causes of Maternal Death:** - Excessive blood loss (hemorrhage) - Infection (sepsis) - High blood pressure (hypertensive disorders like preeclampsia/eclampsia) - Unsafe abortion - Obstructed labor - **Indirect Causes:** Anemia, malaria, heart disease. - **Chronic Contributors:** Anemia, malnutrition, non-communicable diseases (diabetes, hypertension). - **Risk Factors:** Teenage pregnancy, limited access to skilled birth attendance & emergency obstetric care, gaps in prenatal/postnatal service coverage. ### Child Health #### Birth Rate (Crude Birth Rate - CBR) - **Definition:** Number of live births per 1,000 people in a population in one year. - **Reflection:** How fast a population is growing. - **Formula:** $$ \text{CBR} = \frac{\text{Number of live births in a year}}{\text{Mid-year population}} \times 1,000 $$ - **Why "Crude"?** Includes entire population (men, women, children, elderly), not just women of reproductive age. Less precise but simple. - **Uses:** Measure population growth, health planning, national/international comparisons. #### General Fertility Rate (GFR) - **Definition:** Number of live births per 1,000 women of reproductive age (15-49 years) in a year. - **Reflection:** More specific than CBR as it only considers women who can give birth. - **Formula:** $$ \text{GFR} = \frac{\text{Number of live births in a year}}{\text{Number of women aged 15-49 years}} \times 1,000 $$ #### Fetal Death Rate (FDR) - **Definition:** Number of fetuses dying before complete expulsion from the mother (after a specified gestation period) per 1,000 total births in a year. - **Reflection:** Quality of antenatal and intrapartum care. - **What is Fetal Death?** Death of a fetus before birth, with no sign of life after expulsion (includes stillbirths), usually counted after 28 weeks of gestation. - **Formula:** $$ \text{FDR} = \frac{\text{Number of fetal deaths (}\ge\text{28 weeks)}}{\text{Total births}} \times 1,000 $$ - Where: Total births = Live births + Fetal deaths #### Neonatal Death Rate (NDR) - **Definition:** Number of babies dying during the first 28 days of life per 1,000 live births in a given year. - **Reflection:** Quality of antenatal care, delivery care, and immediate newborn care. - **Age Periods:** - Early neonatal: 0-7 days - Late neonatal: 8-28 days - **Formula:** $$ \text{NDR} = \frac{\text{Number of neonatal deaths (0-28 days)}}{\text{Number of live births}} \times 1,000 $$ #### Perinatal Death Rate (PDR) - **Definition:** Measures deaths occurring around the time of birth, combining late fetal deaths (stillbirths) and early neonatal deaths. - **Reflection:** Quality of antenatal care, intrapartum care, and immediate newborn care. - **Included:** - Late fetal deaths (stillbirths) $\ge$ 28 weeks of gestation. - Early neonatal deaths (0-7 days of life). - **Formula:** $$ \text{PDR} = \frac{\text{Late fetal deaths (}\ge\text{28 weeks) + Early neonatal deaths (0-7 days)}}{\text{Total births}} \times 1,000 $$ - Where: Total births = Live births + Late fetal deaths #### Infant Mortality Rate (IMR) - **Definition:** Number of infants dying before completing 1 year of age per 1,000 live births in a given year. - **Reflection:** Most sensitive indicator of maternal health, quality of antenatal/postnatal care, nutrition, sanitation, and immunization. - **Age Periods:** - 0-28 days: Neonatal deaths - 29 days-11 months: Post-neonatal deaths - **Formula:** $$ \text{IMR} = \frac{\text{Number of infant deaths ( ### Nutrition and Growth (Chronic Conditions) - **Stunting:** ~23% of children under 5 (2024) – indicates chronic malnutrition. - **Wasting:** ~6.6% of children under 5 (2024) – indicates acute malnutrition. - **Overweight:** ~6% of children under 5 (2024) – increasing trend. - **Anemia (Micronutrient Deficiency):** ~40% of children under 5, ~37% of pregnant women. ### Chronic and Acute Health Issues in Mothers and Children | Category | Chronic Conditions | Acute Conditions | |------------|------------------------------------------------------|----------------------------------------------------| | **Maternal** | Hypertension, Diabetes, Anemia, Malnutrition | Hemorrhage, Sepsis, Hypertensive crisis, Preterm labor | | **Neonatal** | Congenital disorders, Low birth weight | Birth asphyxia, Neonatal infections, Jaundice | | **Childhood**| Stunting, Developmental delays, Asthma | Pneumonia, Diarrhea, Dengue, Malnutrition-related infections | ### Health System Response and Programs - **MCHN Strategy:** Maternal, Newborn, Child Health and Nutrition. - **Expanded Newborn Screening Program:** Detects 29+ congenital disorders. - **Philippine Plan of Action for Nutrition (PPAN 2023-2028).** - **Kalusugan at Nutrisyon ng Mag-Nanay Act (PA 11148):** Promotes integrated health and nutrition services. - **National Safe Motherhood Program:** Ensures access to quality maternal care. - **Expanded Program on Immunization (EPI):** Maintains coverage for preventable diseases. - **Newborn Care Package (NCP):** Includes immediate drying, skin-to-skin contact, and breastfeeding initiation. ### Key Challenges - Persistent maternal and child mortality (preventable causes). - Inequities in healthcare access (rural vs. urban). - Rising teen pregnancies. - Malnutrition and food insecurity. - Inadequate data/surveillance for congenital/chronic conditions. - Climate-related health impacts (e.g., dengue, heat-related complications). ### Summary of Progress Toward 2030 SDGs | Indicator | Current Status | 2030 Target | Trend | |--------------------------|----------------|-------------|-------------------| | Maternal Mortality | 98/100,000 | 70/100,000 | Off track | | Under-5 Mortality | 26/1,000 | 25/1,000 | Slightly off track| | Stunting | 23% | ### I. Framework for Maternal and Child Nursing This section covers the broader context of MCN. ### A. National Health Situation on Maternal and Child Nursing - **Overview:** The Philippines faces ongoing challenges in maternal and child health outcomes. National goals align with SDGs, aiming to reduce mortality rates by 2030. ### B. Statistics on Maternal and Child Health Nursing #### 1. At-Risk Clients | Indicator/Condition | Latest Statistics (Philippines) | |--------------------------|---------------------------------------------------------------| | Teenage pregnancy | 8.6% of girls aged 15-19 have begun childbearing (NDHS, 2022) | | Inadequate prenatal care | Only ~65% of pregnant women complete 4+ ANC visits (DOH, 2023)| | Maternal anemia | ~37% of pregnant women are anemic (UNICEF-WHO, 2024) | | Low socioeconomic status | Poverty incidence: 22.4% (PSA, 2023) | | Malnutrition among mothers | 1 in 4 women of reproductive age are underweight (FNRI, 2023)| #### 2. High-Risk Clients | Indicator/Condition | Latest Statistics (Philippines) | |---------------------------------------|---------------------------------------------------------------| | Maternal Mortality Ratio (MMR) | 98 deaths per 100,000 live births (PSA, 2023) | | Hypertensive disorders in pregnancy | ~10% of pregnancies (DOH, 2023) | | Gestational diabetes | ~9% of pregnancies (PGH, 2022) | | Preterm birth rate | ~14% (DOH, 2023) | | Low birth weight (LBW) | ~13% of newborns (DOH, 2023) | | Congenital disorders | ~3% of newborns affected (PGH, 2023) | #### 3. Sick Clients | Category | Common Illnesses/Conditions | |----------------------|---------------------------------------------------| | Maternal (sick mothers)| Postpartum hemorrhage, Sepsis, Hypertensive crisis, Eclampsia | | Neonatal (sick newborns)| Birth asphyxia, Neonatal sepsis, Jaundice, Respiratory distress | | Childhood (sick children)| Pneumonia, Diarrhea, Dengue, Malnutrition-related infections | ### C. Genetics and Genetic Counseling #### Table 1. Prevalence of Congenital Disorders by Cause in the Philippines (Screened/Confirmed up to 2024) | Condition | Prevalence (approx.) | |---------------------------------|-------------------------------| | Congenital Hypothyroidism (CH) | ~1 in 2,560 newborns | | Congenital Adrenal Hyperplasia (CAH)| ~1 in 21,016 | | Phenylketonuria (PKU) | ~1 in 122,068 | | Maple Syrup Urine Disease (MSUD)| ~1 in 71,932 | | Organic Acid Disorders | ~1 in 76,093 | | Urea Cycle Defects | ~1 in 649,718 | | Galactosemia | ~1 in 100,918 | | G6PD Deficiency | ~1 in 60 newborns | | Hemoglobinopathies (various forms)| Ranging roughly from ~1 in 2,427 to ~1 in 444,821 | | Cystic Fibrosis | ~1 in 2,111,584 | #### Table 2. Prevalence of Congenital Disorders by Cause in the Philippines (Estimated) | Causes | Estimated Prevalence | |----------------------------------|----------------------| | Dominant single-gene disorders | 7 | | Recessive single gene disorders | 2.3 | | X-linked recessive single-gene disorders| 1.3 | | Chromosomal disorders | 4.2 | | Malformations | 63.9 | ### General Principles Influencing Fetal Growth and Development #### A. Chromosomal Structure - **Chromosomes:** Tightly coiled bundles of DNA found in the nucleus of almost every cell. - **Number:** Humans have 46 chromosomes (23 pairs). - **Alleles:** Pairs of genes for every human trait (one from ovum, one from sperm). - Individuals inherit two alleles for each gene. - Determine physical characteristics (eye color, hair texture, disease susceptibility). - Arise through DNA mutations. - Expressed as **Phenotype** (physical appearance) or **Genotype** (unique traits). - **Autosomes:** 22 pairs of non-sex chromosomes. - **Function:** Carry genes controlling essential proteins for life and most characteristics. - **Abnormalities:** Mutations can lead to conditions like Trisomies (e.g., Down syndrome). - **Testing:** Autosomal DNA testing uses swab/blood samples. - **Sex Chromosomes:** 1 pair (XX for female, XY for male). #### Fertilization - **Process:** Sperm and egg unite to form a zygote (takes ~24 hours). - **Outcome:** Zygote contains genetic info for a new human, undergoes cell division to develop into an embryo, then a fetus. #### B. Nature of Inheritance/Inheritance Patterns - **Genetic Disorders:** Explained by the patterns in which inherited disorders pass from one generation to the next. - **Homozygous:** Has 2 identical genes for a trait. - **Heterozygous:** Has 2 different genes for a trait (one dominant, one recessive). - **Dominant Gene:** Expressed even if only one copy is present. - **Recessive Gene:** Expressed only if both alleles carry it. - **Mendelian Laws:** Predict inheritance of characteristics and genetic disorders. #### Principle of Mendelian Inheritance - **Law of Segregation:** Two alleles for each gene separate into different gametes during meiosis. - **Law of Independent Assortment:** Inheritance of one gene doesn't affect the inheritance of another gene. - **Law of Dominance:** When two different alleles are present, only the dominant one is expressed. #### C. Chromosomal Inheritance Disorder **Modes of Inheritance:** - Autosomal Dominant - Autosomal Recessive - X-Linked Dominant - X-Linked Recessive - Y-Linked - Multifactorial ##### Autosomal Dominant Disorder - **Key:** A single copy of a mutated gene is enough to cause the disorder. - **Characteristics:** Child of affected parent has 50% chance of inheriting; dominant traits don't skip generations. - **Examples:** - **Familial Hypercholesterolemia:** High LDL cholesterol, early heart attacks. - **Myotonic Dystrophy:** Muscle weakness, myotonia (difficulty relaxing muscles). - **Huntington's Disease (HD):** Progressive breakdown of nerve cells, physical/mental deterioration. - **Neurofibromatosis:** Tumors on nerve tissue. - **Polycystic Kidney Disease (PKD):** Clusters of cysts in kidneys. - **Achondroplasia:** Short-limbed dwarfism ("without cartilage formation"). ##### Autosomal Recessive Disorder - **Key:** Two copies of a mutated gene are required to cause the disorder. - **Characteristics:** Child of two unaffected carriers has 25% chance of inheriting; aren't always seen in every generation. - **Examples:** - **Thalassemia:** Abnormal/inadequate hemoglobin production. - **Cystic Fibrosis (CF):** Mutation in CFTR gene, affects lungs/pancreas. Carriers have one normal, one mutated gene. - **Galactosemia:** Inability to process galactose, can cause liver damage, sepsis, death. - **Sickle Cell Disease:** Misshapen (sickle-shaped) red blood cells due to hemoglobin gene mutation, causes pain. - **Hemochromatosis:** Faulty gene (HFE) causes excessive iron absorption. ##### X-Linked Dominant - **Key:** A mutated gene on the X chromosome causes the condition. - **Characteristics:** - Males with mutated X chromosome will have the condition. - Females with one mutated X are usually unaffected (due to having another normal X). - Affected males are more common than affected females. - All daughters of affected males will have the condition. - **Examples:** - **Fragile X Syndrome (FXS):** Mild-to-moderate intellectual disability due to FMR1 gene changes. - **Vitamin D-Resistant Rickets:** Body doesn't respond to Vitamin D, symptoms range in severity. - **Alport's Syndrome:** Damages kidneys, ears, eyes due to collagen IV gene mutation. ##### X-Linked Recessive - **Key:** A mutated gene on the X chromosome causes the condition, but two copies are needed for females to be affected, while males only need one. - **Characteristics:** - Females with one mutated X chromosome will have the condition (rare, usually carriers). - Males with one mutated X chromosome will have the condition. - Males are more commonly affected. - **Examples:** - **Hemophilia A:** Deficiency in clotting factor VIII, preventing blood clotting. - **Hemophilia B (Christmas Disease):** Deficiency in clotting factor IX. - **Color Blindness/Deficiency:** Inability to see certain colors due to light-sensitive cell issues. - **Duchenne Muscular Dystrophy (DMD):** Progressive muscle degeneration due to dystrophin protein alteration, mainly affects boys. ##### Y-Linked - **Key:** Disorders are only passed from father to son. - **Characteristics:** Y-linked diseases are rare as the Y chromosome is small and carries few genes. - **Examples:** - **Hypertrichosis of the Ears:** Excessive hair growth on the outer rim of the ear. - **Webbed Toes:** Second and third toes connected by a web-like structure. - **Porcupine Man:** Skin thickens, darkens, scaly, rough, and bristle-like. - **Infertility:** Condition making reproduction difficult or impossible. ##### Multifactorial - **Key:** Caused by a combination of genetic and environmental factors. - **Genetic Factors:** Combination of genes from both parents. - **Environmental Factors:** Nutrition, lifestyle, alcohol, tobacco, pollution, illness, medicines. - **Examples:** - **Congenital Heart Defects:** Problems with heart structure at birth. - **Clubfoot (Talipes Equinovarus - CTEV):** Foot pointed inward/downward at birth. - **Neural Tube Defects (NTDs):** Neural tube doesn't close properly (first month of pregnancy). - **Spina Bifida:** Fetal spinal column doesn't close completely. - **Anencephaly:** Baby born without parts of the brain. - **Pyloric Stenosis:** Narrowing of stomach opening to small intestines (pylorus), occurs 0-6 months, causes projectile vomiting. - **Cleft Lip:** Opening/split in the upper lip. - **Cleft Palate:** Opening/split in the roof of the mouth. ##### Mitochondrial Inheritance - **Key:** Passed down from mother to all her children (both sons and daughters). - **Characteristics:** If mother has mtDNA mutation, she passes it to all children. Daughters can then pass it on, but sons cannot. - **Examples:** - **Leber's Hereditary Optic Neuropathy (LHON):** Vision loss due to mtDNA mutations damaging optic nerve cells. - **Leigh Syndrome:** Neurological symptoms including muscle weakness, loss of motor skills, seizures. ### Chromosomal Abnormalities Genetic conditions from an abnormal number or arrangement of chromosomes. #### Types: 1. **Numerical Abnormalities:** Missing or extra chromosomes. - **Monosomy:** Missing one chromosome from a pair (e.g., Turner Syndrome, X0). - **Trisomy:** Extra copy of a chromosome (e.g., Down Syndrome, Trisomy 21; Edwards Syndrome, Trisomy 18; Patau Syndrome, Trisomy 13). - **Polyploidy:** More than two sets of chromosomes (e.g., Triploidy). 2. **Structural Abnormalities:** Change in chromosome structure (missing, extra, or switched parts). 3. **Sex Chromosome Abnormalities:** Abnormality in X or Y chromosomes (e.g., Klinefelter Syndrome XXY, Turner Syndrome X0). #### Contributing Factors: - Exposure to teratogens. - Advanced maternal age at conception. #### Specific Chromosomal Disorders: - **Trisomy 21 (Down Syndrome):** Extra chromosome at position 21. - **Trisomy 18 (Edwards Syndrome):** Extra chromosome at position 18. Severe, affects body development. - **Trisomy 13 (Patau Syndrome):** Extra chromosome at position 13. Serious, rare. - **Klinefelter Syndrome (Genotype XXY):** Male has an extra X chromosome. - **Turner Syndrome (Genotype X0):** Female with missing or partially missing X chromosome. ### Nursing Process Overview for Genetic Principles #### Assessment - **Health History:** Focus on couple's risk for inherited disorder. - Relevant preliminary genetic history. - Ethnic background. - General medical history. - **Laboratory and Diagnostic Studies.** #### Nursing Diagnosis - Knowledge deficit. - Decisional conflict. - Anticipatory grieving. #### Planning and Outcome Identification - Parents educated on genetic problems, risks, treatment options. - Parents receive emotional support during genetic counseling. #### Implementation - **Provide Education:** - Describe parent's risk for inherited disorder. - Provide sufficient and correct information about the genetic problem. - Explain genetic testing required. - Provide information on possible treatment. - Provide information on available resources. - **Provide Emotional Support:** - Identify counseling needs. - Provide risk-appropriate health care and counseling. - Assist coping with test results. - Refer to appropriate providers/support groups. - Serve as liaison between genetic counselor and family. #### Outcome Evaluation - Parents demonstrate adequate knowledge. - Parents show positive coping and make informed choices. ### Principles of Counseling - **Principle of Individualization:** Each person is unique; understand and respect their characteristics. - **Principle of Purposeful Expression of Feelings:** Create an atmosphere for free expression of feelings, building trust. - **Principle of Controlled Emotional Involvement:** Be sensitive but not overly emotional; empathize without being overwhelmed. - **Principle of Acceptance:** Accept clients as they are, with their strengths and weaknesses. - **Principle of Non-Judgmental Attitude:** Avoid preconceived notions; present options impartially. - **Principle of Client Self-Determination:** Respect client's right to make their own choices, offering options/alternatives. - **Principle of Confidentiality:** Safeguard all shared information. #### Refer to Guidance Counselor or Psychiatrist When: - Problem is more serious than you can handle. - You are too busy or stressed. - You've helped all you can, but more is needed. - Your personal feelings interfere with objectivity. - Client asks for information/assistance you cannot provide. ### Genetic Counseling #### Purposes: - Provide accurate information on inherited disorders. - Reassure those concerned about inheritance. - Allow informed decisions about future reproduction. - Educate on inherited disorders and inheritance process. - Offer support to those affected. #### Goals: - Enable informed reproductive decisions. - Provide psychological support. - Inform clients about defects. - Communicate risk of transmitting defects to future children. #### Who Benefits from Genetic Testing/Counseling (Referral): - Couples with a child with a congenital disorder. - Couples with relatives having a genetic disorder. - Individuals known to be balanced translocation carriers. - Individuals with inborn chromosomal disorders. - Consanguineous couples. - Women >35, men >45. - Couples from ethnic backgrounds with known specific illnesses. #### Indication for Prenatal Genetic Screening: - Parent is carrier/affected by chromosomal/metabolic disorder. - Family history of genetic disorder (especially in susceptible ethnic backgrounds). - Previous child with congenital abnormality/multiple anomalies (no chromosomal studies). - Advanced maternal age. - History of spontaneous abortion. - Willingness to interrupt pregnancy if abnormal fetus is detected. ### Screening for Genetic Traits and Disease #### Goal of Screening: - Prevent tragic genetic diseases. - Offer reproductive options to at-risk couples. - Accurate screening on education and advocacy of physicians and nurses for people of reproductive age. #### Specific Tests: - Karyotyping - Heterozygote screening - Maternal serum alpha-fetoprotein screen - Triple screening - Chorionic villi sampling - Amniocentesis - Percutaneous umbilical blood sampling - Sonography - Fetoscopy #### Nursing Responsibilities in Genetic Screening: - Assess for signs/symptoms of genetic disorders. - Offer support to individuals seeking genetic counseling. - Help with reproductive genetic testing procedures. - **Instrumental in:** - Alerting couples to procedures. - Explaining genetic screening tests. - Assisting with wait for results. - Assisting with values clarification, planning, decision-making. - Serving as liaison and referrer to other healthcare providers.