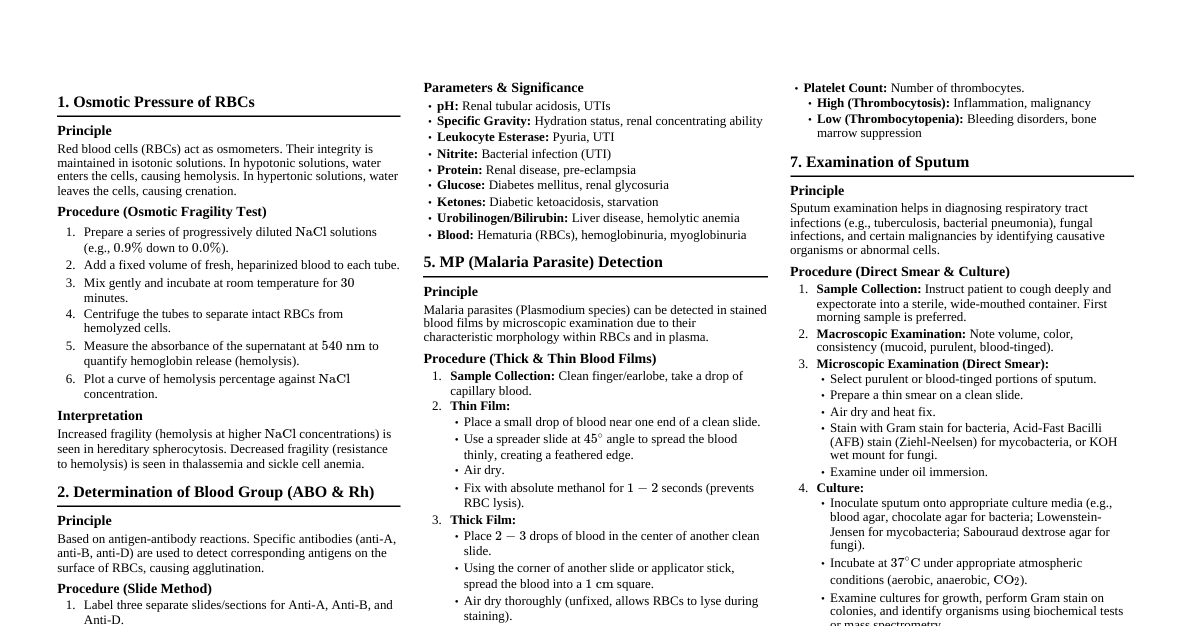
1. Osmotic Pressure of RBCs Principle Red blood cells (RBCs) act as osmometers. Their integrity is maintained in isotonic solutions. In hypotonic solutions, water enters the cells, causing hemolysis. In hypertonic solutions, water leaves the cells, causing crenation. Procedure (Osmotic Fragility Test) Prepare a series of progressively diluted $\text{NaCl}$ solutions (e.g., $0.9\%$ down to $0.0\%$). Add a fixed volume of fresh, heparinized blood to each tube. Mix gently and incubate at room temperature for $30$ minutes. Centrifuge the tubes to separate intact RBCs from hemolyzed cells. Measure the absorbance of the supernatant at $540 \text{ nm}$ to quantify hemoglobin release (hemolysis). Plot a curve of hemolysis percentage against $\text{NaCl}$ concentration. Interpretation Increased fragility (hemolysis at higher $\text{NaCl}$ concentrations) is seen in hereditary spherocytosis. Decreased fragility (resistance to hemolysis) is seen in thalassemia and sickle cell anemia. 2. Determination of Blood Group (ABO & Rh) Principle Based on antigen-antibody reactions. Specific antibodies (anti-A, anti-B, anti-D) are used to detect corresponding antigens on the surface of RBCs, causing agglutination. Procedure (Slide Method) Label three separate slides/sections for Anti-A, Anti-B, and Anti-D. Place a drop of Anti-A serum on the 'A' section, Anti-B on 'B', and Anti-D on 'D'. Add a drop of the patient's blood (whole blood or $2-5\%$ RBC suspension) to each drop of antiserum. Mix thoroughly with separate applicators for each section. Gently rock the slide for up to $2$ minutes. Observe for agglutination macroscopically. Interpretation Agglutination with Anti-A only: Blood Group A Agglutination with Anti-B only: Blood Group B Agglutination with Anti-A and Anti-B: Blood Group AB No agglutination with Anti-A or Anti-B: Blood Group O Agglutination with Anti-D: Rh Positive ($\text{Rh}^+$) No agglutination with Anti-D: Rh Negative ($\text{Rh}^-$) 3. Determination of Blood Glucose Principle (Glucose Oxidase Method) Glucose oxidase catalyzes the oxidation of glucose to gluconic acid and hydrogen peroxide. Peroxidase then catalyzes the reaction of hydrogen peroxide with a chromogen (e.g., o-toluidine) to produce a colored product, the intensity of which is proportional to glucose concentration. Procedure (Spectrophotometric Method) Collect blood sample (fasting or random). Use fluoride-oxalate tubes to prevent glycolysis. Centrifuge to obtain plasma/serum. Prepare reagents: Glucose oxidase, peroxidase, chromogen. Set up three tubes: Blank, Standard, Test. Add reagents and plasma/serum according to kit instructions. Incubate at $37^\circ\text{C}$ for a specified time (e.g., $10-15$ minutes). Stop the reaction (e.g., with sulfuric acid). Measure absorbance of Standard and Test samples at a specific wavelength (e.g., $505 \text{ nm}$) against the Blank. Calculate glucose concentration: $$ \text{Glucose (mg/dL)} = \frac{\text{Absorbance of Test}}{\text{Absorbance of Standard}} \times \text{Concentration of Standard} $$ 4. Examination of Urine by Dipstick Principle Dipsticks are impregnated with various chemical reagents that react with specific urine components, producing color changes indicative of their presence and concentration. Procedure Collect a fresh, well-mixed, mid-stream urine sample in a clean container. Dip the reagent strip completely into the urine, ensuring all pads are immersed. Immediately remove the strip, dragging it against the rim of the container to remove excess urine. Hold the strip horizontally to prevent color run-over between pads. Wait for the specified reaction times for each pad (usually $30$ seconds to $2$ minutes). Compare the color changes on the strip pads to the color chart provided on the reagent strip container. Record results for each parameter (e.g., pH, specific gravity, leukocytes, nitrite, protein, glucose, ketones, urobilinogen, bilirubin, blood). Parameters & Significance pH: Renal tubular acidosis, UTIs Specific Gravity: Hydration status, renal concentrating ability Leukocyte Esterase: Pyuria, UTI Nitrite: Bacterial infection (UTI) Protein: Renal disease, pre-eclampsia Glucose: Diabetes mellitus, renal glycosuria Ketones: Diabetic ketoacidosis, starvation Urobilinogen/Bilirubin: Liver disease, hemolytic anemia Blood: Hematuria (RBCs), hemoglobinuria, myoglobinuria 5. MP (Malaria Parasite) Detection Principle Malaria parasites (Plasmodium species) can be detected in stained blood films by microscopic examination due to their characteristic morphology within RBCs and in plasma. Procedure (Thick & Thin Blood Films) Sample Collection: Clean finger/earlobe, take a drop of capillary blood. Thin Film: Place a small drop of blood near one end of a clean slide. Use a spreader slide at $45^\circ$ angle to spread the blood thinly, creating a feathered edge. Air dry. Fix with absolute methanol for $1-2$ seconds (prevents RBC lysis). Thick Film: Place $2-3$ drops of blood in the center of another clean slide. Using the corner of another slide or applicator stick, spread the blood into a $1 \text{ cm}$ square. Air dry thoroughly (unfixed, allows RBCs to lyse during staining). Staining (Giemsa Stain): Dilute Giemsa stain $1:10$ or $1:20$ with buffered water (pH $6.8-7.2$). Stain thin film for $10-15$ minutes. Stain thick film for $20-30$ minutes. Rinse gently with buffered water. Air dry completely. Microscopic Examination: Examine thin film under oil immersion ($100\times$) for species identification (parasite morphology, infected RBC morphology). Examine thick film under oil immersion ($100\times$) for parasite detection and quantification (higher sensitivity). Scan at least $100$ fields. Interpretation Identify characteristic forms of Plasmodium trophozoites, schizonts, and gametocytes. Differentiate species (e.g., P. falciparum , P. vivax , P. ovale , P. malariae ) based on morphology, size, and number of merozoites. 6. Complete Blood Count (CBC) Principle Automated hematology analyzers use various technologies (e.g., impedance, light scatter, flow cytometry) to count and differentiate blood cells and measure hemoglobin. Manual methods involve microscopy and hemocytometers. Procedure (Automated Analyzer) Collect venous blood in an $\text{EDTA}$ (lavender top) tube. Gently invert the tube several times to ensure proper mixing with anticoagulant. Place the sample tube into the automated hematology analyzer. The analyzer aspirates a small volume of blood. Blood is diluted, lysed, and passed through various detection chambers. Results are generated for multiple parameters. Key Parameters & Significance White Blood Cell (WBC) Count: Total number of leukocytes. High: Infection, inflammation, leukemia Low: Immunosuppression, bone marrow failure WBC Differential: Percentage of different WBC types (Neutrophils, Lymphocytes, Monocytes, Eosinophils, Basophils). Neutrophilia: Bacterial infection Lymphocytosis: Viral infection Eosinophilia: Allergies, parasitic infection Red Blood Cell (RBC) Count: Total number of erythrocytes. High: Polycythemia Low: Anemia Hemoglobin (Hb): Oxygen-carrying protein in RBCs. Low: Anemia Hematocrit (Hct): Volume percentage of RBCs in blood. Low: Anemia Mean Corpuscular Volume (MCV): Average RBC volume. Low (Microcytic): Iron deficiency anemia, thalassemia High (Macrocytic): Vitamin $\text{B}_{12}$/folate deficiency, liver disease Mean Corpuscular Hemoglobin (MCH) / Concentration (MCHC): Average Hb per RBC / concentration. Low (Hypochromic): Iron deficiency anemia Red Cell Distribution Width (RDW): Variation in RBC size. High: Anisocytosis, early iron deficiency Platelet Count: Number of thrombocytes. High (Thrombocytosis): Inflammation, malignancy Low (Thrombocytopenia): Bleeding disorders, bone marrow suppression 7. Examination of Sputum Principle Sputum examination helps in diagnosing respiratory tract infections (e.g., tuberculosis, bacterial pneumonia), fungal infections, and certain malignancies by identifying causative organisms or abnormal cells. Procedure (Direct Smear & Culture) Sample Collection: Instruct patient to cough deeply and expectorate into a sterile, wide-mouthed container. First morning sample is preferred. Macroscopic Examination: Note volume, color, consistency (mucoid, purulent, blood-tinged). Microscopic Examination (Direct Smear): Select purulent or blood-tinged portions of sputum. Prepare a thin smear on a clean slide. Air dry and heat fix. Stain with Gram stain for bacteria, Acid-Fast Bacilli (AFB) stain (Ziehl-Neelsen) for mycobacteria, or KOH wet mount for fungi. Examine under oil immersion. Culture: Inoculate sputum onto appropriate culture media (e.g., blood agar, chocolate agar for bacteria; Lowenstein-Jensen for mycobacteria; Sabouraud dextrose agar for fungi). Incubate at $37^\circ\text{C}$ under appropriate atmospheric conditions (aerobic, anaerobic, $\text{CO}_2$). Examine cultures for growth, perform Gram stain on colonies, and identify organisms using biochemical tests or mass spectrometry. Perform antibiotic susceptibility testing if significant bacterial growth is present. Interpretation Gram Stain: Identify morphology of bacteria (cocci, bacilli) and Gram reaction (positive/negative). AFB Stain: Presence of acid-fast bacilli suggests tuberculosis. Culture: Identify specific pathogenic bacteria, fungi, or mycobacteria. Cytology (if requested): Presence of malignant cells. 8. Examination of Fecal Specimen Principle Fecal examination (Stool microscopy) is crucial for diagnosing gastrointestinal infections, malabsorption syndromes, and screening for colorectal cancer by detecting parasites, pathogenic bacteria, blood, fat, or abnormal cells. Procedure (Macroscopic, Microscopic, Chemical) Sample Collection: Collect a fresh sample in a clean, dry, leak-proof container. Avoid contamination with urine or toilet water. Macroscopic Examination: Observe color, consistency (formed, loose, watery), presence of mucus, blood, or worms. Microscopic Examination: Wet Mount: Mix a small amount of stool with saline and iodine on separate slides. Cover with coverslip. Examine under $10\times$ and $40\times$ for ova, cysts, larvae of parasites, WBCs, RBCs, yeast cells, fat globules. Stained Smear (e.g., Methylene Blue, Gram Stain): For specific cellular elements or bacteria if indicated. Chemical Tests: Fecal Occult Blood Test (FOBT): Detects hidden blood (guaiac-based or immunochemical). Fecal Fat: Sudan III stain for neutral fats and fatty acids (malabsorption). pH: Indicates carbohydrate malabsorption. Culture (if bacterial infection suspected): Inoculate stool onto selective media (e.g., MacConkey, Salmonella-Shigella agar, Campy-BAP). Incubate and identify pathogenic bacteria (e.g., Salmonella, Shigella, Campylobacter, E. coli O157:H7 ). Interpretation Parasites: Identification of specific protozoan cysts/trophozoites or helminth eggs/larvae. WBCs/RBCs: Indicates inflammation or bleeding in GI tract. Occult Blood: GI bleeding (ulcers, polyps, cancer). Increased Fat: Malabsorption. Pathogenic Bacteria: Identified by culture and susceptibility testing. 9. Culturing Blood (Blood Culture) Principle Blood culture is used to detect and identify microorganisms (bacteria, fungi) circulating in the bloodstream (bacteremia, fungemia), which can lead to sepsis. Blood is inoculated into specialized culture media designed to promote microbial growth. Procedure Site Preparation: Crucial for preventing contamination. Clean venipuncture site thoroughly with $70\%$ alcohol, then with an antiseptic (e.g., $2\%$ chlorhexidine or povidone-iodine) using a concentric scrubbing motion. Allow to air dry for the recommended time. Blood Collection: Collect $20-30 \text{ mL}$ of blood (adults) per venipuncture, dividing it into $2-3$ sets from different sites if possible, or into aerobic and anaerobic bottles from the same site. Each set typically consists of one aerobic and one anaerobic bottle. Use a sterile needle and syringe or a blood collection system. Inoculation: Aseptically remove the plastic cap from the blood culture bottles and disinfect the rubber septum with alcohol. Inject the collected blood into the appropriate bottles (typically $8-10 \text{ mL}$ per bottle). Mix the bottles gently by inversion. Incubation: Transport bottles to the laboratory promptly. Incubate in an automated blood culture system at $37^\circ\text{C}$ for up to $5-7$ days (longer for specific organisms like fungi). Automated systems continuously monitor for $\text{CO}_2$ production or other metabolic changes indicating microbial growth. Positive Culture Work-up: If a bottle signals positive, perform a Gram stain directly from the bottle fluid. Subculture onto appropriate agar media (e.g., blood agar, chocolate agar, MacConkey agar). Identify the organism using biochemical tests, mass spectrometry, or molecular methods. Perform antibiotic susceptibility testing. Interpretation Positive blood culture indicates bacteremia or fungemia. The identified organism and its susceptibility profile guide antimicrobial therapy. Differentiate true pathogens from contaminants based on organism type, number of positive bottles, and patient clinical status.